Long-term use of PPIs linked to stomach cancer
Posted: 31 October 2017 | Dr Zara Kassam (European Pharmaceutical Review) | No comments yet
The long-term use of proton pump inhibitors, a class of drugs commonly used to treat acid reflux, is linked to the risk of developing stomach cancer…
The long-term use of proton pump inhibitors (PPIs), a class of drugs commonly used to treat acid reflux, is linked to a more than doubling in the risk of developing stomach cancer.
The risk rose in tandem with the dose and duration of treatment following the elimination of Helicobacter pylori, the bacteria implicated in the development of stomach cancer, the findings show.
Eliminating H pylori from the gut significantly lowers a person’s risk of developing stomach cancer. But a substantial proportion of those in whom treatment is successful still go on to develop the disease, the third leading cause of cancer death in the world.
Previously published research has found an association between PPI use and heightened stomach cancer risk, but it was unable to factor in the potential role of H pylori itself, so undermining the strength of the findings.
To try and get around this, the researchers compared the use of PPIs with another type of drug used to dampen down acid production called histamine H2 receptor antagonists (H2 blockers) in 63,397 adults treated with triple therapy–a combination of a PPI and two antibiotics to kill off H pylori over 7 days–between 2003 and 2012.
They were subsequently monitored until they either developed stomach cancer, died, or the study ended, whichever came first. The average monitoring period lasted 7.5 years. During this time, 3271 (5%) people took PPIs for an average of nearly three years; and 21,729 took H2 blockers.
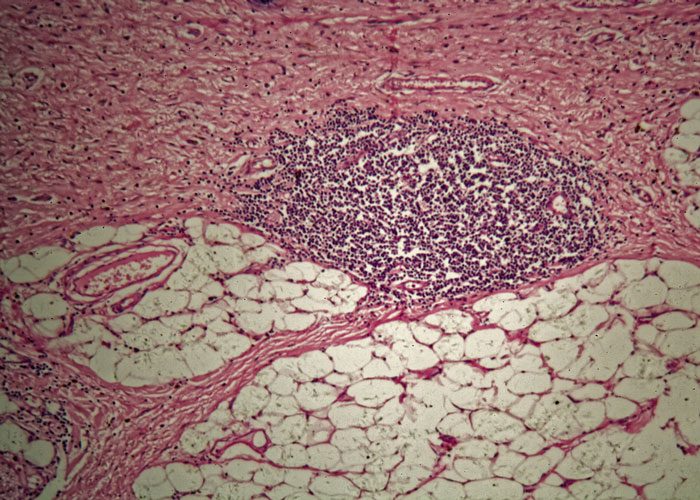
In all, 153 (0.24%) people developed stomach cancer after triple therapy. None tested positive for H pylori at the time, but all had long-standing gastritis (inflammation of the stomach lining).
Taking PPIs was associated with a more than doubling (2.44) in the risk of developing stomach cancer while taking H2 blockers was not associated with any such heightened risk.
The average time between triple therapy and the development of stomach cancer was just under 5 years.
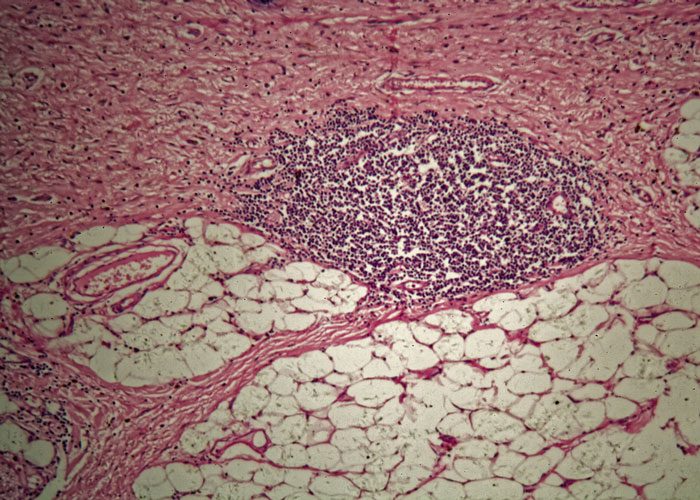
More frequent use was associated with greater risk, with daily use linked to a more than quadrupling in risk (4.55) compared with weekly use.
And the longer PPIs were used, the greater was the risk of developing stomach cancer, rising to 5-fold after more than a year, to more than 6-fold after two or more years, and to more than 8-fold after three or more years.
This is an observational study, so no firm conclusions can be drawn about cause and effect, and PPIs are generally considered safe, say the researchers.
But recent research has linked their long-term use to various unwanted effects, including pneumonia, heart attack, and bone fracture, they point out, adding that PPIs are known to stimulate the production of gastrin, a powerful growth factor.
The “clear dose-response and time response trend” in the use of PPIs and stomach cancer risk, prompt them to suggest that doctors “should exercise caution when prescribing long-term PPIs…even after successful eradication of H plyori.”
The research has been published online in the journal Gut.