Abeona enrols first Phase 2 patient following successful Phase 1 Epidermolysis trial
Posted: 27 September 2016 | | No comments yet
Also known as “Butterfly skin” syndrome, epidermolysis bullosa (EB) is a rare genetic skin disease that is caused by the absence of a gene (COL7A1)…
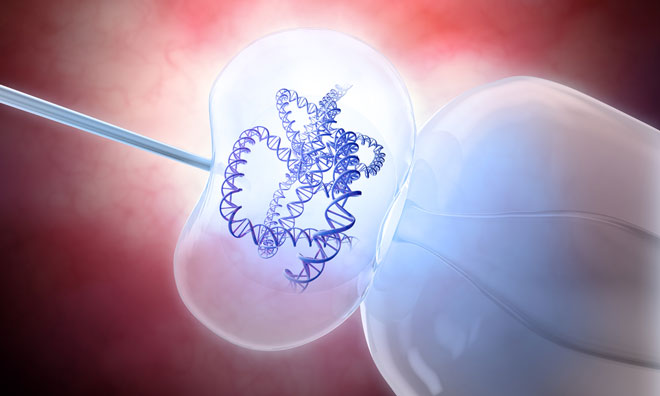
Abeona Therapeutics has enrolled their first patient in the Phase 2 portion of the clinical trial for EB-101, gene-corrected skin grafts, the company’s lead gene therapy program for patients suffering with recessive dystrophic epidermolysis bullosa (RDEB), a severe form of epidermolysis bullosa (EB).
Also known as “Butterfly skin” syndrome, RDEB is a rare genetic skin disease that is caused by the absence of a gene (COL7A1) which encodes a protein known as type VII collagen (C7). Patients with RDEB develop large, painful blisters and chronic wounds from minor trauma to their skin and currently there are no FDA approved treatments for RDEB. The Phase 1/2 clinical trial with gene-corrected skin grafts has shown promising wound healing and safety in patients with RDEB.
Trial expansion
Investigators at Stanford University are now expanding enrolment to adolescent and adult patients for the Phase 1/2 trial to determine the safety and efficacy of COL7A1 gene-corrected grafts on wound healing efficacy.
“Treating the first patient in the Phase 2 portion of the EB-101 study marks a significant milestone for Abeona’s efforts to advance our lead EB program. Results from the ongoing Phase 1/2 clinical data demonstrates that EB-101 is well tolerated in patients with RDEB, a very debilitating rare skin disease associated with high rates of morbidity and mortality, with no approved FDA treatment options,” said Timothy Miller PhD President and CEO of Abeona Therapeutics.
Epidermolysis Bullosa is a group of devastating, life-threatening genetic skin disorders impacting children that is characterised by skin blisters and erosions all over the body. One of the most severe forms, recessive dystrophic epidermolysis bullosa (RDEB), is characterised by chronic skin blistering, open and painful wounds, joint contractures, oesophageal strictures, pseudo syndactyly, corneal abrasions and a shortened life span. Along with the life- threatening infectious complications associated with this disorder, many individuals often develop an aggressive form of squamous cell carcinoma (SCC).




