Gene test could predict spread of breast cancer to the brain
Posted: 21 October 2015 |
Research has found that women whose breast cancer had begun to spread and who tested positive in the αB-crystallin test were three times more likely to have disease that spread to the brain…
Women with particularly aggressive forms of breast cancer could be identified by a test that predicts whether the disease is likely to spread to the brain.
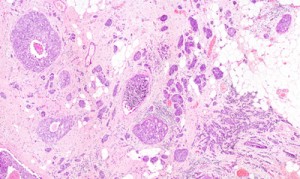
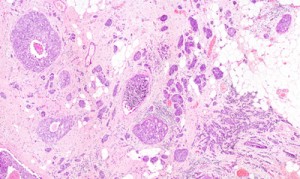
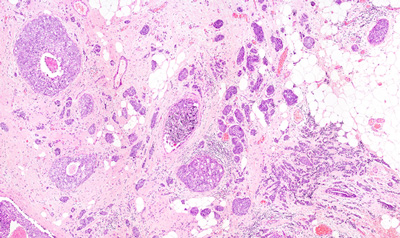
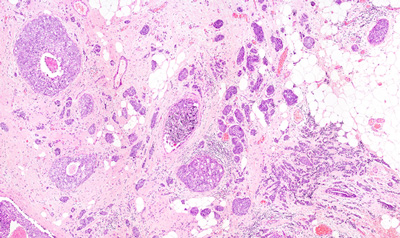
An analysis of almost 4,000 patients with breast cancer found that testing for high activity in a particular gene called alpha beta (αB)-crystallin could pick out women who were at greater risk of developing secondary brain tumours compared to women who tested negative.
In fact, a research team found that women whose breast cancer had begun to spread and who tested positive in the αB-crystallin test were three times more likely to have disease that spread to the brain than those who tested negative.
Women can live for years with breast cancer that has begun to spread around the body – but the exception is spread to the brain, which usually indicates a woman is in her last few months of life.
In the study, the researchers analysed 969 breast cancer tumours which ultimately spread, or metastasised, to new sites in the body, from a database of almost 4,000 breast cancers from the British Columbia Cancer Agency. 141 had spread first to the brain. Some 127 scored positive for αB-crystallin, and 842 negative – with those testing positive three times more likely to have spread first to the brain.
αB-crystallin linked with a significantly higher risk of death
In a further analysis of all 4,000 cases, αB-crystallin was also linked with a significantly higher risk of death – with 36% of women with αB-crystallin positive cancer, compared to 25% with αB-crystallin negative, dying within ten years of diagnosis.
Study co-leader Dr Maggie Cheang, Senior Staff Scientist at The Institute of Cancer Research, London, said, “Spread of breast cancer to the brain is unfortunately very dangerous, and usually leads to death within months. It’s important to find new ways to identify women who are most at risk of their cancer spreading to the brain, so that doctors can work out which women might need more intensive or new treatments to try to keep their cancer at bay for longer.
“Our study linked a positive score in this test with quicker spread to the brain, and importantly showed the factor we were measuring is providing information on patient outcome independently of other biomarkers already measured in the clinic.
“The test needs further development before it will be ready for routine clinical use, but ultimately the first use of this type of test could be to identify opportunities for women with advanced specific types of breast cancer – such as triple negative – to enter clinical trials of new treatments.”




