Biogen Idec presents positive interim results from Phase 1b study of investigational Alzheimer’s Disease treatment aducanumab
Posted: 23 March 2015 |
Biogen Idec has announced data from the Phase 1b study of aducanumab, in which the drug demonstrated positive results in patients with prodromal or mild AD…


Biogen Idec has announced data from a pre-specified interim analysis of PRIME, the Phase 1b study of aducanumab (BIIB037), in which aducanumab demonstrated an acceptable safety profile and positive results on radiologic and clinical measurements in patients with prodromal or mild Alzheimer’s disease (AD).
These data were presented at the 12th International Conference on Alzheimer’s and Parkinson’s Diseases and Related Neurological Disorders in Nice, France.
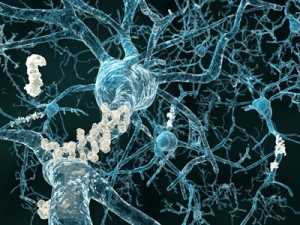
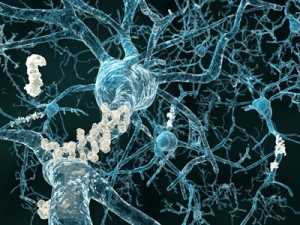
Treatment with aducanumab produced a dose- and time-dependent reduction of amyloid plaque in the brain. Amyloid plaque is believed to play a key role in the development of the symptoms of AD. In exploratory analyses, a dose-dependent, statistically significant effect of slowing clinical decline was observed on the Mini Mental State Examination (MMSE) and Clinical Dementia Rating (CDR) scales.
Aducanumab demonstrated a statistically significant reduction on amyloid plaque
“This is the first time an investigational drug for Alzheimer’s disease has demonstrated a statistically significant reduction on amyloid plaque as well as a statistically significant slowing of clinical impairment in patients with prodromal or mild disease,” said Alfred Sandrock, M.D., Ph.D., group senior vice president and chief medical officer at Biogen Idec. “Based on these results, we are advancing the aducanumab clinical program to Phase 3 with plans to initiate enrollment later this year.”
PRIME Study
PRIME is an ongoing Phase 1b randomized, double-blind, placebo-controlled, multiple-dose study evaluating the safety, tolerability, pharmacokinetics (PK) and pharmacodynamics (PD) of aducanumab in patients with prodromal or mild AD.
This interim analysis of PRIME reflects data for 166 patients, up to week 54 in the placebo (n=40), 1 mg/kg (n=31), 3 mg/kg (n=33) and 10 mg/kg (n=32) dose arms, and up to week 30 data for the 6 mg/kg (n=30) dose arm.
Radiologic Results for Amyloid Plaque
In patients receiving aducanumab, a dose- and time-dependent reduction of amyloid plaque was observed over 54 weeks of treatment.
PET imaging using the radiotracer florbetapir1, which binds to amyloid plaque, was used to measure plaque levels in the brain. A composite standardized uptake value ratio (SUVR) of six regions of the brain –frontal, parietal, lateral temporal, sensorimotor, anterior and posterior cingulate – was calculated at baseline, at 26 weeks and at 54 weeks using whole cerebellum as a reference.
In the placebo arm, the SUVR was virtually unchanged at 26 and 54 weeks. Aducanumab treatment resulted in a statistically significant reduction of amyloid plaque in the 3 mg/kg [average change of -0.087, p<0.01)], 6 mg/kg [-0.143 (p<0.001)] and 10 mg/kg [-0.205 (p<0.001)] dose arms compared to placebo at 26 weeks. Amyloid plaque levels were reduced by -0.030 in the 1 mg/kg arm, which was not significant.
At week 54, a statistically significant reduction of amyloid plaque was observed in the 3 mg/kg [-0.139 (p<0.001)] and 10 mg/kg [-0.266 (p<0.001)] dose arms. The reduction of amyloid plaque in the 1 mg/kg (-0.056) arm was not significant. The 6 mg/kg arm is ongoing and the week 54 data will become available at a later date.
Clinical Results
The effect of aducanumab on AD-related impairment was measured using the MMSE and Clinical Dementia Rating sum of boxes (CDR-SB). The MMSE is used to assess a patient’s cognitive status and the CDR-SB characterizes a patient’s cognitive and functional performance.
On the MMSE, patients in the placebo group worsened by an average of 3.14 at one year, whereas the decline was 2.21 in the 1 mg/kg arm, 0.75 in the 3 mg/kg arm and 0.58 in the 10 mg/kg arm. Relative to placebo, the 3 mg/kg and 10 mg/kg doses demonstrated a statistically significant slowing of cognitive decline on the MMSE, both with p-values <0.05.
On the CDR-SB, patients in the placebo group worsened by an average of 2.04 at one year. In comparison, the worsening was 1.70 in the 1 mg/kg arm, 1.33 in the 3 mg/kg arm and 0.59 in the 10 mg/kg arm. Relative to placebo, the 10 mg/kg showed a statistically significant slowing of clinical decline on the CDR-SB with p-value <0.05.
Pharmacokinetic activity and exposure were linear with dose. Treatment-emergent immunogenicity, which occurred in approximately 3 percent of patients, was transient and without apparent effect on aducanumab PK.
Safety Results
Aducanumab demonstrated an acceptable safety and tolerability profile in this analysis. The most frequently reported treatment-related serious adverse event (SAE) and adverse event (AE) was ARIA (amyloid-related imaging abnormalities).
Based on MRI scans, the incidence of ARIA-E (edema) was dose- and apolipoprotein E4-(ApoE4) status-dependent. In general, the onset of ARIA-E was observed early in the course of treatment and was asymptomatic or with mild, transient symptoms. The majority of patients with ARIA-E continued treatment and did so at a lower dose.
In ApoE4 carriers, the incidence of ARIA-E was 5 percent in the 1 mg/kg and 3 mg/kg arms, 43 percent in the 6 mg/kg arm and 55 percent in the 10 mg/kg arm. In ApoE4 non-carriers, the incidence of ARIA-E was 9 percent, 11 percent and 17 percent in the 3 mg/kg, 6 mg/kg and 10 mg/kg aducanumab arms, respectively; no cases were reported in the 1 mg/kg arm.
In ApoE4 carriers, the incidence of patients who developed ARIA-E and discontinued treatment was 5 percent in the 1 mg/kg arm, 10 percent in the 6 mg/kg arm, and 35 percent in the 10 mg/kg arm. There were no discontinuations in the 3 mg/kg arm. In ApoE4 non-carriers, the incidence of patients who developed ARIA-E and discontinued treatment was 11 percent in the 6 mg/kg arm and 8 percent in the 10 mg/kg arm. There were no discontinuations in the 1 mg/kg and 3 mg/kg arms.
Headache occurred in 22 percent of patients receiving aducanumab compared to 5 percent in the placebo groups and appeared to be dose-dependent. Three deaths were reported in the time period of this analysis, two in the placebo group and one in the 10 mg/kg study arm; none were considered to be treatment related. Other AEs and SAEs were consistent with what is typically observed in the study population.
- Amyvid™ (florbetapir) is a trademark of Eli Lilly and Company.
For more information on Biogen Idec, please visit www.biogen.com.




