First-in-class combination therapy authorised for endometriosis
Posted: 5 September 2024 | Catherine Eckford (European Pharmaceutical Review) | No comments yet
The three-in-one oral daily tablet provides an additional treatment option to help women in the UK manage their endometriosis-associated pain.
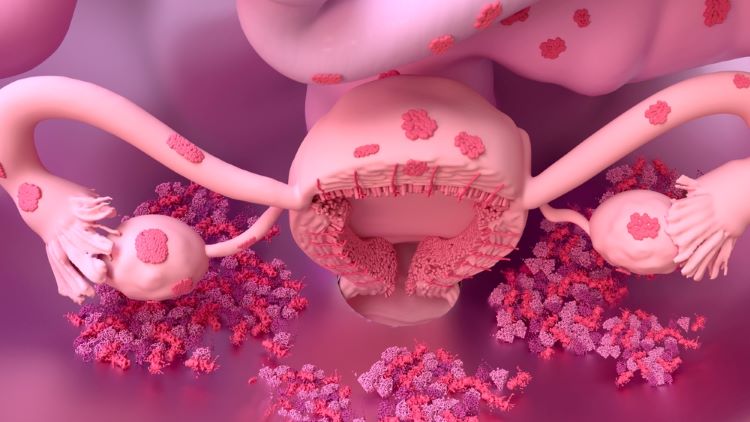
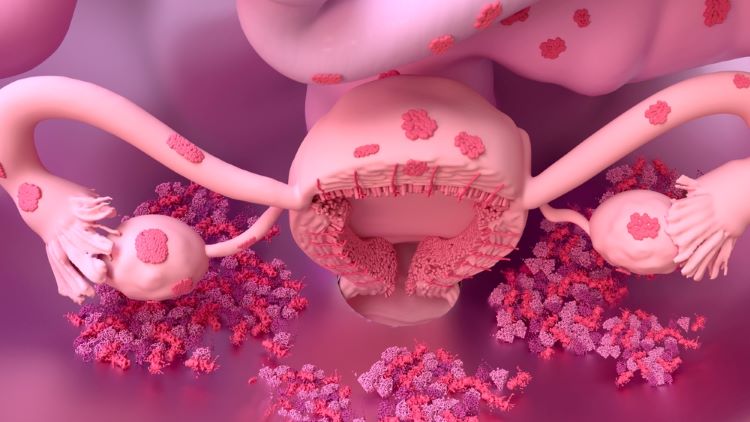
The Medicines and Healthcare Products Regulatory Agency (MHRA) has licenced the first treatment (oral gonadotropin-releasing hormone [GnRH] receptor antagonist) in a new class of medicines for women in the UK with endometriosis. Relugolix combination therapy, Ryeqo (relugolix 40mg, estradiol 1mg, and norethisterone acetate 0.5mg), is authorised to treat endometriosis symptoms in adults.
The oral therapy is indicated for women of reproductive age who have had prior medical or surgical treatment for their endometriosis.
“With limited treatments available in the UK, relugolix combination therapy which is taken in a single, once daily tablet may help people take control of their endometriosis-associated pain,” explained Professor Andrew Horne, Director of the Centre for Reproductive Health, University of Edinburgh.
What data is the authorisation of relugolix combination therapy based on?
The MHRA licence is based on outcomes from the Phase III SPIRIT programme (SPIRIT 1 and SPIRIT 2). Significantly more women achieved pain reduction with the combination therapy compared to placebo at 24 weeks, according to the trial data.
“With limited treatments available in the UK, relugolix combination therapy which is taken in a single, once daily tablet may help people take control of their endometriosis-associated pain”
For instance, in SPIRIT 1, 75 percent of women responded to relugolix combination therapy for their dysmenorrhoea compared to 27 percent given placebo treatment, Gedeon Richter noted.
Similarly, SPIRIT 2, there were 75 percent of dysmenorrhoea responders. In the placebo arm, this statistic totalled 30 percent.
In SPIRIT 1, response to relugolix combination therapy for non-menstrual pelvic pain (NMPP) symptoms was reported to be 59 percent. There were 40 percent of participants treated with placebo who responded to the combination therapy, data showed.
Comparatively, in SPIRIT 2, there were 66 percent of NMPP responders versus 43 percent in the placebo arm.
Furthermore, a long-term extension study up to 80 weeks found that the relugolix combination therapy enabled participants to experience reduced dysmenorrhoea and NMPP over a two-year period.
“We believe this authorisation will be a welcome step for redefining care. We are now engaging with the relevant health authorities throughout the UK with a view to securing NHS reimbursement as soon as possible,” shared David Jordan, Medical Director UK and Ireland, Gedeon Richter.
Gedeon Richter stated that availability of relugolix combination therapy on the NHS is anticipated for publication in 2025.
Related topics
Clinical Development, Clinical Trials, Data Analysis, Drug Development, Drug Markets, Drug Safety, Industry Insight, oral therapeutic candidate, Regulation & Legislation, Research & Development (R&D), Therapeutics
Related organisations
Gedeon Richter, The Medicines and Healthcare products Regulatory Agency (MHRA)
Related drugs
oral drugs, relugolix combination therapy, Ryeqo (relugolix/estradiol/norethisterone acetate)









