Phase III results: Once daily olodaterol* Respimat® provides effective and sustained improvements in lung function in patients with COPD1-3
Posted: 9 September 2013 | | No comments yet
Data from two 48 week Phase III studies involving more than 3,000 patients…


Data from two 48 week Phase III studies involving more than 3,000 patients show that olodaterol Respimat® in addition to usual care provides statistically significant improvements in lung function vs. usual care alone in patients with COPD (GOLD stages 2-4).1-3
Usual care background therapy included long- and short-acting anticholinergics, short-acting beta agonists, inhaled corticosteroids and xanthines.
Efficacy data from the trials demonstrate that once-daily olodaterol Respimat® has a rapid onset of action within 5 minutes after the first dose2 and maintains lung function over 24 hours.4
What does this mean for patients?
Compared to usual care alone, lung function improvements with once-daily olodaterol Respimat® resulted in a statistically significant, greater number of COPD patients achieving clinically meaningful improvements in their quality of life, as reflected by a decrease of more than 4 units in the St. George’s Respiratory Questionnaire (SGRQ)† total score.3
“Despite advances in the treatment of COPD, there remains a significant need to reduce the burden of COPD on patients’ lives. We are excited about these data because we see that the lung function improvements shown with olodaterol translate into patient related benefits over and above those seen with usual care, which reflects the need in a real-world situation,” said Dr Gary T Ferguson of the Pulmonary Research Institute of Southeast Michigan, Livonia, Michigan, US.
“It is important to pay careful attention to permitted background therapies when interpreting the results of any bronchodilator study in COPD. A clinical trial where the active drug is compared against placebo in the absence of other background maintenance bronchodilator therapies is how COPD bronchodilator studies have been done. This methodology will more likely show a greater bronchodilator response vs. placebo than when other bronchodilator therapies are allowed in the placebo treatment group,” Dr. Ferguson concluded.
The addition of olodaterol Respimat® once-daily over 48 weeks provided statistically significant improvements in lung function vs. usual care alone (p<0.05) that were comparable to those shown with formoterol Aerolizer® 12 µg twice-daily.2
A responder analysis showed that more patients treated with olodaterol had a decrease in SGRQ total score greater than the minimal clinically important difference (MCID) of 4 units compared with usual care alone (P<0.001). For formoterol 12 μg, there was no significant difference compared with usual care alone in the number of patients with a decrease in SGRQ total score greater than the MCID (P=0.4621).
Safety data from the four 48-week Phase III parallel pivotal studies: two comparing olodaterol Respimat® vs. usual care alone and two comparing olodaterol Respimat® vs. formoterol Aerolizer® twice-daily, showed that, overall, the frequency of adverse events (AE) experienced with olodaterol was comparable to both placebo and the active comparator formoterol.5 The most common AE was COPD exacerbations.5
“We are committed to bringing olodaterol Respimat® to patients worldwide who need an additional treatment option. Boehringer Ingelheim has designed olodaterol Respimat® as a combination partner for tiotropium to provide additional bronchodilation in the maintenance treatment of COPD. We are currently undertaking a large global Phase III clinical trial programme in COPD – TOviTO® – to investigate the efficacy and safety of a combination of tiotropium with olodaterol in a once-daily fixed-dose combination using the Respimat® inhaler,” said Professor Klaus Dugi, Corporate Senior Vice President Medicine at Boehringer Ingelheim.
“Olodaterol Respimat® has the potential to be an effective new treatment option for COPD patients and represents the next step in a series of important advances from our robust pipeline of respiratory treatments. This pipeline is driven by our passion for finding innovative ways to address the unmet needs of the millions of patients whose ability to lead a full life is disrupted by lung diseases. With these new treatment options, Boehringer Ingelheim continues to maintain leadership in COPD and to provide potential innovative solutions in other respiratory areas such as asthma, idiopathic pulmonary fibrosis (IPF) and lung cancer,” Professor Dugi concluded.
About olodaterol
Olodaterol is a highly selective, long-acting beta2-agonist (LABA) for the once-daily maintenance bronchodilator treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema. It is approved for use in the treatment of COPD in Canada and Russia; approval and regulatory reviews by health authorities in the US, Europe and other countries are pending.
Boehringer Ingelheim is developing olodaterol as a combination partner for tiotropium to provide additional bronchodilation in the maintenance treatment of patients with COPD. Combining a long-acting anticholinergic (LAMA), such as tiotropium, and a LABA has the potential to deliver increased bronchodilatory benefits in COPD symptoms and consistency of treatment response, compared to monotherapy.14
About SPIRIVA® (tiotropium bromide) in COPD
SPIRIVA®, a long-acting anticholinergic medication, is the first inhaled maintenance treatment to provide significant and sustained improvements in lung function with once-daily dosing. SPIRIVA® positively impacts the clinical course of COPD, helping to change the way patients live with their disease.6 Since SPIRIVA® was first introduced over ten years ago, it has become the most prescribed maintenance treatment for COPD worldwide. SPIRIVA® helps COPD patients breathe more easily by opening narrowed airways and helping to keep them open for 24 hours. It works through targeting of a dominant reversible mechanism of COPD – cholinergic bronchoconstriction.
SPIRIVA® is delivered via HandiHaler®, a breath-actuated, single-dose dry powder inhaler, or by the SPIRIVA® Respimat® Soft MistTM Inhaler.
About Respimat® Soft MistTM Inhaler
Developed by Boehringer Ingelheim, Respimat® Soft MistTM Inhaler (SMI) is a new generation inhaler delivering a unique slow-moving Soft MistTM that allows gentle inhalation – making it easy to inhale,7-9 and is preferred by patients compared to other currently available inhalers.10,11
About COPD
COPD is a chronic lung syndrome, including chronic bronchitis and emphysema, dominated by progressive air flow limitation. Major symptoms are shortness of breath, chronic cough and sputum, and repeated exacerbations.12
COPD is caused by long-term inhalation exposure to pollutants and noxious particles, most commonly cigarette smoke.12
As COPD progresses, lung function declines and physical activity may become severely limited, disrupting the patient’s ability to lead a full life, interfering with everyday tasks and participation in family routines.12 This can lead to people feeling, anxious, isolated and depressed.12,13
Bronchodilator medications are central to symptom management in COPD12 and inhaled bronchodilators are recommended in guidelines as first choice for the initial pharmacological management of COPD.12
For patients who remain symptomatic on one bronchodilator, the combination of two bronchodilators with different modes of action – a LAMA with a LABA – has the potential to be more effective in improving airflow and in helping patients with COPD to achieve better outcomes, compared to existing treatment options.14
References
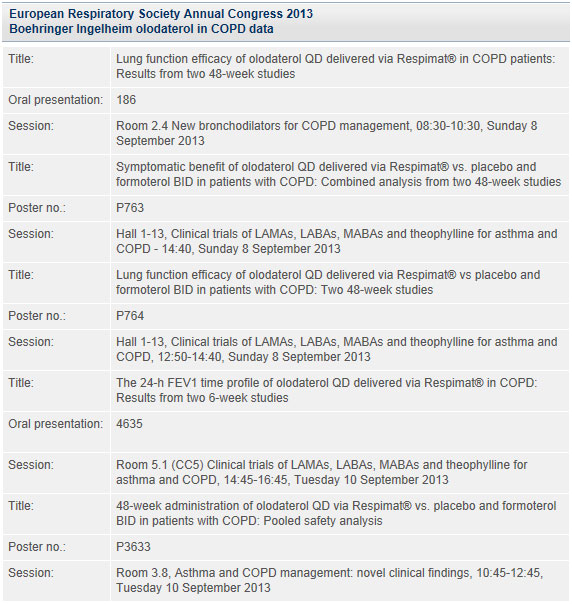
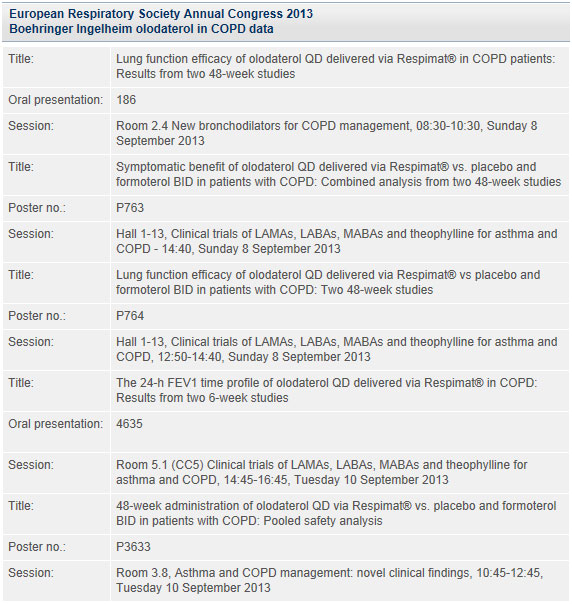
- Ferguson GT, Feldman GJ, Hofbauer P, et al. Lung function efficacy of olodaterol QD delivered via Respimat® in COPD patients: results from two 48-week studies. ERS 2013 oral presentation 186.
- Koch A, Pizzichini E, Hamilton A, et al. Lung function efficacy of olodaterol QD delivered via Respimat® vs placebo and formoterol BID in patients with COPD: two 48-week studies. ERS 2013 poster no. P764.
- Koch A, Paggiaro P, Hamilton A, et al. Symptomatic benefit of olodaterol QD delivered via Respimat® vs placebo and formoterol BID in patients with COPD: combined analysis from two 48-week studies. ERS 2013 poster no. P763.
- Lange P, Aumann J-L, Derom E, et al. The 24-h FEV1 time profile of olodaterol QD delivered via Respimat® in COPD: results from two 6-week studies. ERS 2013 oral presentation 4635.
- McGarvey L, Koch A, Sachs P, et al. 48-week administration of olodaterol QD via Respimat® vs placebo and formoterol BID in patients with COPD: pooled safety analysis. ERS 2013 poster no. P3633.
- Vincken W, van Noord JA, Greefhorst APM, et al. Improved health outcomes in patients with COPD during 1 year’s treatment with tiotropium. Eur Respir J 2002;19:209-216.
- Dhand R. Aerosol plumes: slow and steady wins the race. J Aerosol Med 2005;18(3):261-263.
- Hochrainer D, Hölz H, Kreher C, et al. Comparison of aerosol velocity and spray duration of Respimat® Soft MistTM inhaler and pressurized metered dose inhalers. J Aerosol Med 2005;18(3):273-282.
- Kardos P, Golisch W, Wolf K. New SoftMistTM Inhaler is effective and easy to use in patients with asthma and COPD. Eur Respir J 2005; 26 (Suppl 49): 338s.
- Hodder R, Reese PR, Slaton T. Asthma patients prefer Respimat® Soft MistTM Inhaler to Turbohaler®. Int J Chronic Obstruct Pulm Dis 2009;4:225-232.
- Schürmann W, Schmidtmann S, Moroni P, et al. Respimat® Soft MistTM inhaler versus hydrofluoroalkane metered dose inhaler: patient preference and satisfaction. Treatm Respir Med 2005;4:53-61.
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2013).
- Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD –current understanding, unanswered questions and research needs. Chest 2008;134;43S-56S.
- Cazzola M, Molimard M. The scientific rationale for combining long-acting β2-agonists and muscarinic antagonists in COPD. Pulm Pharmacol Ther 2010;23:257-267.
*Olodaterol (Striverdi®) Respimat® is approved for use in COPD in Canada and Russia. Approval and regulatory reviews by health authorities in the US, Europe and other countries are pending.
†A 50-item questionnaire developed to measure health status (quality of life) in patients with COPD covering breathlessness in daily life and ability to exercise, as well as anxiety and depression. A decrease of 4 units in the SGRQ total score has been identified as the minimum clinically significant change




