Intratumoural viral delivery improves glioblastoma survival
Posted: 17 May 2023 | Catherine Eckford (European Pharmaceutical Review) | No comments yet
“Injecting a virus into a patient’s brain tumour” combined with immunotherapy improved glioblastoma survival outcomes in a clinical trial.
An engineered oncolytic virus (DNX-2401) targeting glioblastoma (GBM) cells combined with subsequent immunotherapy using intratumoural delivery, gave a 52.7 percent 12-month overall survival (OS) rate for patients with recurrent GBM.
According to the Phase I/II trial results published in Nature Medicine, this is higher than the prespecified efficacy threshold of 20 percent. Twenty percent of patients with recurrent GBM remained alive for at least three years, and tumour reduction in complete responders continued for more than a year.
Viral therapy as an oncology treatment
DNX-2401 is a cold virus engineered to selectively target and invade GBM cells while avoiding normal cells.
“Injecting a virus into a patient’s brain tumour is disruptive science” and is different to the current standard of care, stated Dr Juan Fueyo, Professor of Neuro-Oncology, Division of Cancer Medicine, MD Anderson Cancer Center, University Of Texas, US.
The viral therapy “aims to awaken the patient’s immune system and trigger a healing from within,” Dr Fueyo commented. “After injection, patients that respond well develop inflammation inside the tumour, triggering an immune response that first kills the virus.”
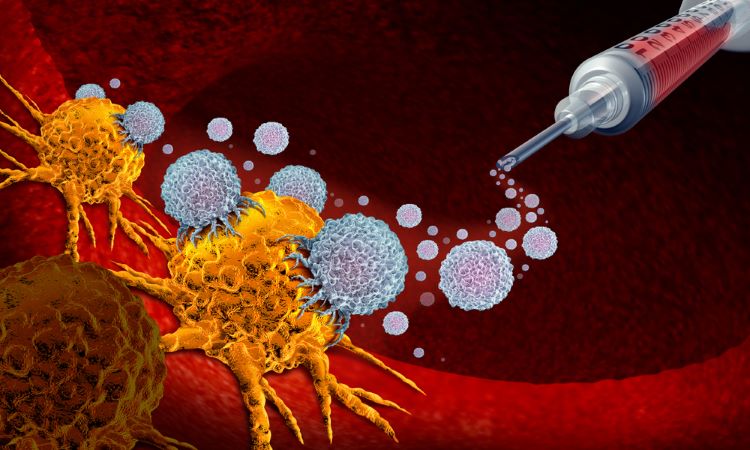
Dr Fueyo added: “The continued immune reaction, stimulated by additional immunotherapy, destroys the cancer cells in a tightly regulated way without the side effects common to chemotherapy or radiation therapy.”
“Our previous trial demonstrated that not only does the virus act by killing cancer cells directly, it also effectively activates the innate immune system to convert these immunologically cold tumours into hot tumours,” stated co-corresponding author Dr Frederick Lang, Chair of Neurosurgery at MD Anderson Cancer Center, University Of Texas, in the US.
“This led us to evaluate a combination with checkpoint inhibitors, which we now see can improve survival outcomes in a subset of patients,” noted Dr Lang.
While immune checkpoint blockade has improved outcomes in other cancer types to glioblastoma, in recurrent GBM, immune cell infiltration is not possible. This makes it difficult to treat the cancer with immunotherapy.
An increase in PD-1 checkpoint expression was seen following the treatment via intratumoural delivery. This suggested that the immune system may be primed to respond to anti-PD-1 immunotherapy.
Novel device opens blood-brain barrier to deliver chemotherapy
Intratumoural delivery
The current trial was designed to evaluate the combination of intratumoural DNX-2401 followed by intravenous pembrolizumab therapy.
The study enrolled 49 patients with recurrent GBM from several institutions between September 2016 to January 2019. The median age of patients was 53 years and 41 percent were women.
In the trial, 98 percent of patients were treated with one dose of DNX-2401 after biopsy. This was followed by pembrolizumab given one week later.
The combination achieved a clinical benefit, defined as stable disease or better, in 56.2 percent of the patients.
Five patients had objective responses and two experienced tumour reduction of 80 percent or more at six months follow-up. By 18 months, these two patients had a complete response without evidence of disease progression.
Potential of smart viruses
“Our studies using this ‘smart virus’ are ongoing, but we are encouraged that we continue to see a small number of patients who have a very dramatic eradication of the tumour,” added Dr Candelaria Gomez-Manzano, Professor of Neuro-Oncology, Division of Cancer Medicine, MD Anderson Cancer Center at the University Of Texas, US.
The study was supported by Merck & Co.
Clinical trials currently are underway using mesenchymal stem cells (MSC) to deliver more of the smart virus to the tumour and more widely through the tumour. Future clinical trials will evaluate alternate treatments, such as checkpoint inhibitors or CAR T-cell therapy, in combination with DNX-2401.
Related topics
Anti-Cancer Therapeutics, Big Pharma, Clinical Development, Clinical Trials, Drug Delivery Systems, Drug Development, Drug Safety, Drug Targets, Immunotherapy, Research & Development (R&D), Therapeutics, Viruses
Related organisations
Merck & Co, The University of Texas MD Anderson Cancer Center
Related drugs
Related people
Dr Candelaria Gomez-Manzano, Dr Frederick Lang, Dr Juan Fueyo