First patients given lab-grown blood cell transfusion
Posted: 7 November 2022 | Catherine Eckford (European Pharmaceutical Review) | No comments yet
The second-ever patient has been transfused with lab-grown red blood cells in a clinical trial, promising an effective treatment for patients.
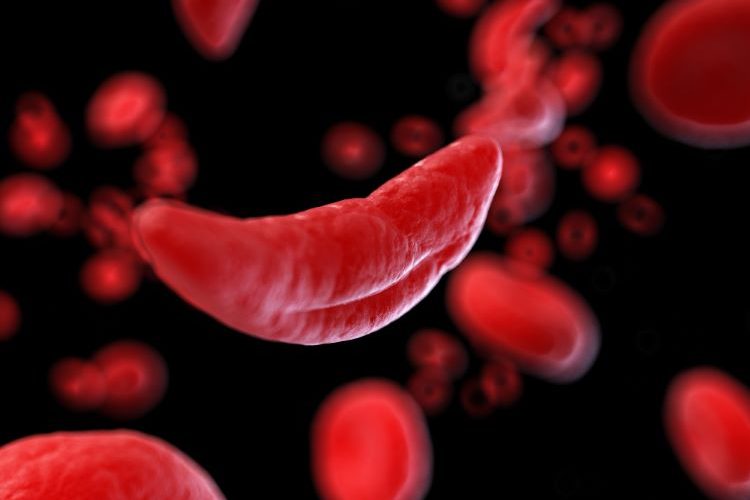
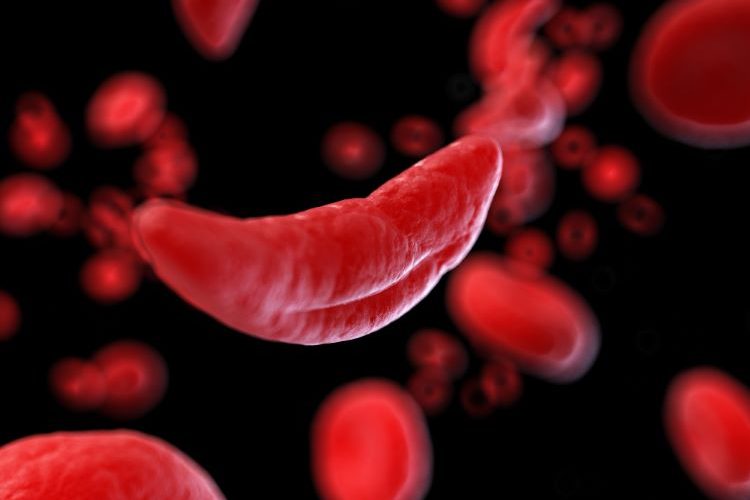
Lab-grown blood cells have been transfused into a second patient in the world’s first-of-a-kind clinical trial, opening up future treatments for blood disorders such as sickle cell if found safe and effective.
Stem cells from blood donors were separated and grown to produce modified red blood cells at NHS Blood and Transplant (NHSBT) Advanced Therapies Unit in Bristol.
The study is run by the National Institute for Health and Care Research (NIHR) Blood and Transplant Research Unit in Red Blood Cell Products from the NHSBT and University of Bristol.
RESTORE, the randomised, controlled clinical trial investigated the lifespan of the modified cells compared to standard red blood cell infusions from the same donor. Similar transfusions with standard donated red cells contain cells of varying ages. However, as the lab-grown blood cells are fresh, researchers expect the therapy will perform better. They anticipate patients who need regular blood transfusions could require fewer transfusions over time. The new therapy should reduce their risk of severe complications from iron overload, a danger of frequent blood transfusions.
Patients in the trial did not encounter problematic side effects.
Manufactured red blood cells in clinical trials
At least 10 trial participants with rare blood types or complex transfusion needs will receive two mini transfusions, at least four months apart. The quantity of lab-grown blood cells being infused can vary, however it is around five to 10ml. Researchers plan to administer one transfusion of standard blood cells plus one of lab-grown blood cells. This will help determine if the modified cells last longer than standard cells made in the body.
John James OBE, Chief Executive of the Sickle Cell Society commented: “This research offers real hope for those difficult to transfuse sickle cell patients who have developed antibodies against most donor blood types.”
Dr Farrukh Shah, Medical Director of Transfusion for NHS Blood and Transplant stated: “Patients who need regular or intermittent blood transfusions may [as a] result develop antibodies against minor blood groups, which makes it harder to find donor blood which can be transfused without the risk of a potentially life-threatening reaction.”
Neil O’Brien, Minister of State for Health shared: “This research… represents a breakthrough for patients and means treatment could be transformed for those with diseases including sickle cell.”
The part-NIHR funded study also collaborated with experts from the University of Cambridge, Guy’s and St Thomas’ NHS Foundation Trust, NIHR Cambridge Clinical Research Facility and Cambridge University Hospitals NHS Foundation Trust.
Related topics
Biologics, Biopharmaceuticals, Clinical Development, Clinical Trials, Drug Development, Immunotherapy, Research & Development (R&D), Stem Cells, Therapeutics
Related organisations
NHS Blood and Transplant (NHSBT) Cellular and Molecular Therapies, Sickle Cell Society, University of Bristol