Live from CPhI: ‘Gut microbiome therapy to be approved in the next two years’
Posted: 3 November 2022 | CPhI | No comments yet
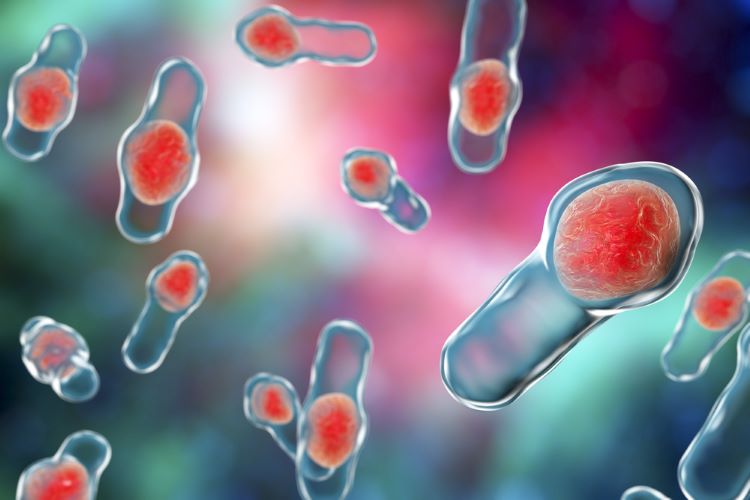
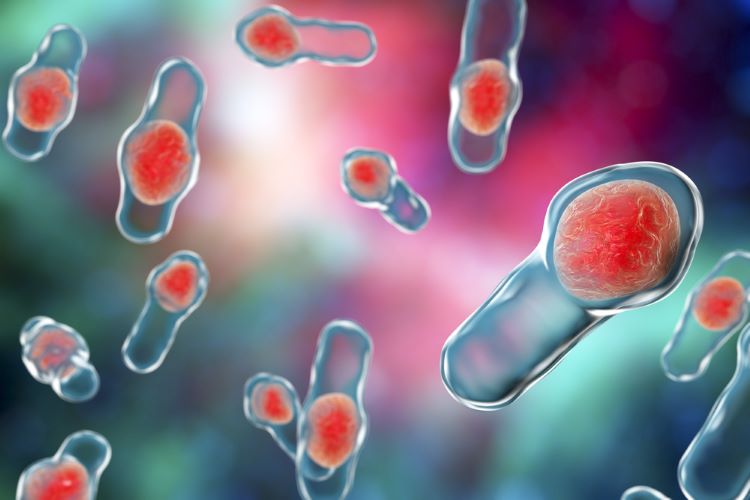
The promise of microbiome-based therapeutics is rapidly progressing towards real world applications as treatment of recurrent Clostridium difficile using faecal microbiota transplant edges towards a BLA.
Speaking live from CPhI Frankfurt, Christian Roghi, Director of Microbiome Solutions, predicted microbiome therapy will be the next big breakthrough in novel therapies, rivalling discoveries like mABs, siRNA and CAR T cells.
“We are seeing huge interest in microbiome research, especially in the last five years. There have been a large number of publications describing both the science and the potential benefits of a healthy microbiome,” added Roghi.
In total there are some 524 microbiome therapeutics – 48 percent in pre-clinical development and 42 percent in clinical development – with live biotherapeutics products dominating (177 therapeutics).
Regulating microbiome therapies
However, before a commercial approval can be found, the challenges are manifold as the entire regulatory framework needs to be established and matured. For example, the design of clinical trials, the IP laws – how can you patent live microbial environments – and safety profiles. Yet, despite these considerable barriers to commercial applications, there are a number of candidates in late-stage trials, with Roghi boldly predicting these will be approved within the next two years.
Looking deeper, Roghi explained that a faecal microbiota transplant (FMT) is the process of transferring faecal bacteria and other microbes from a healthy individual into another individual and is now a recognised as an effective treatment for C. diff infection.
However, longer term, the benefits of microbiome-based therapeutics extend far beyond these initial applications, with implications for skin-brain and inter-organ microbial communication.
This is because microbes residing inside and on a healthy human body, play a massive role in the health of the individual. Microbial therapy harnessing this unique natural phenomenon creates the therapeutic potential to treat a plethora of patients, with indications as diverse as anxiety, stress, liver infections and even cancer. For example, it has recently been established that the tumour microbiome environment affects the efficacy of anti-cancer therapies. This, potentially, points to a future use of microbial markers for each patient so that therapeutic interventions can be personalised to the microbiome of the specific patient.
The long road ahead
Roghl stated that with over 33 treatments in late-stage treatments we are soon to see one progress to market authorisation, specifically those under development from Ferring Pharmaceuticals and Seres Therapeutics – both of which are targeting C. diff infections.
Yet, despite these great strides the biology and modes of action of these therapies remain largely unestablished, and we are only at the beginning of ‘scratching the surface’ of their potential. For now, researchers speculate that it’s a multimodal effect related to restoring of microbial diversity in the patient.
Roghl described that microbiome therapies ‘can transform non-responders to responders in certain cancers, for example, in the treatment of melanoma to list just one’.
Related topics
Anti-Cancer Therapeutics, Biologics, Biopharmaceuticals, Microbiology, Microbiomes, Research & Development (R&D), Therapeutics