ITM licenses targeted radionuclide therapy candidate
Posted: 26 October 2022 | Catherine Eckford (European Pharmaceutical Review) | No comments yet
The targeted radionuclide therapy for glioblastoma is administered into a tumour cavity via a reservoir post-surgery and standard post-operative therapy.
A novel targeted radionuclide therapy candidate for malignant glioblastoma, LuCaFab (ITM-31), will be licensed to ITM Isotope Technologies Munich SE (ITM), a German radiopharmaceutical firm.
ITM will hold exclusive rights to LuCaFab, including Intellectual Property patent, use and manufacturing knowledge. The licence is based on option and co-operation agreements announced in January 2022, which aimed to advance the therapeutic into clinical development.
LuCaFab is suited as an additional therapy for glioblastoma, post-treatment to prevent future tumour growth. “…We believe that targeted radiotherapy, particularly ITM-31 can make a significant impact for patients by selectively eliminating tumour remnants post-surgery,” stated Steffen Schuster, CEO of ITM.
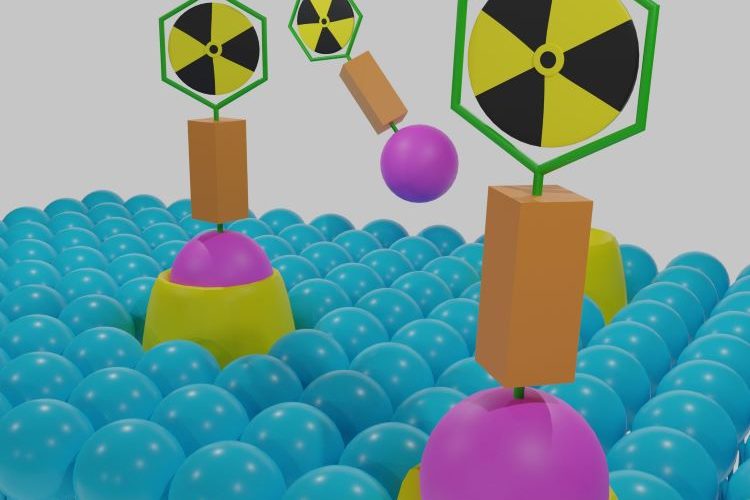
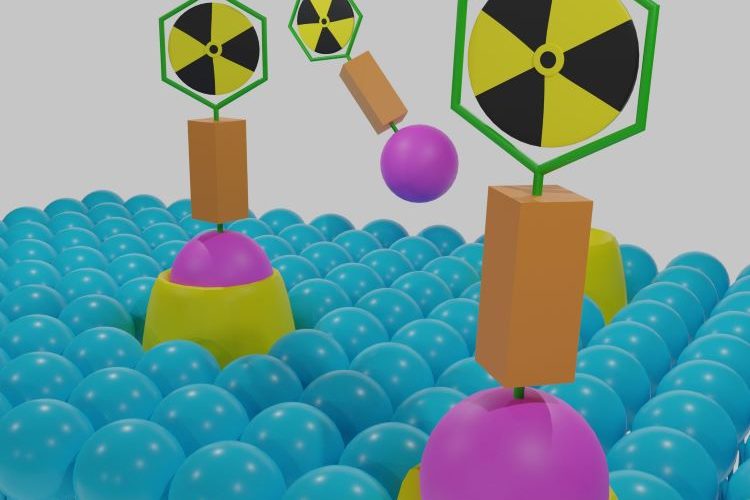
The therapy targets CA XII, an antigen highly expressed on the surface of glioblastoma cells but is not found on healthy glial cells, a type of brain cells. LuCaFab consists of ITM-31, a carbonic anhydrase XII (CA XII)-specific antibody Fab fragment paired with the radioisotope non-carrier-added Lutetium-177 (n.c.a. 177Lu, EndolucinBeta®).
The drug is administered using Targeted Radionuclide Therapy – a relatively new class of cancer treatment that directs radiation into a tumour, exposing normal tissue to a minimal amount of radiation.
Targeted radionuclide therapy links a radioisotope to a targeting molecule with the ability to recognise and bind to tumour cells. The radioisotope decays at the tumour site and releases a therapeutic quantity of ionising radiation, destroying the tumour.
LuCaFab is administered into a tumour cavity via a reservoir post-surgery and standard post-operative therapy (intracavitary). From here, LuCaFab migrates precisely into local tissue (avoiding healthy cells) and binds to glioblastoma cells, which are then irradiated.
Glioblastoma is a rare cancer, one of the most aggressive types of solid brain tumours. Data estimates there are only three to five news cases for every 100,000 people per year. As the tumour cells penetrate into surrounding tissue, 90 percent of cancerous relapse occurs in the site surrounding the original tumour. This makes development of a suitable treatment of primary importance for the industry.