Baricitinib and remdesivir reduce time to recovery in COVID-19 patients
Posted: 18 January 2021 | Victoria Rees (European Pharmaceutical Review) | No comments yet
A clinical trial in hospitalised COVID-19 patients has demonstrated that baricitinib and remdesivir reduce time to recovery.


A clinical trial involving hospitalised COVID-19 patients has found that a combination of the drugs baricitinib and remdesivir reduce time to recovery. The study was co-ordinated at the University of Texas Health San Antonio and University Health, US, and was conducted at roughly 100 sites globally.
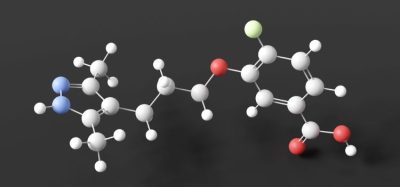
The Adaptive COVID-19 Treatment Trial 2 (ACTT-2), which compared the combination therapy versus remdesivir paired with an inactive placebo, was supported by the US National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH). Remdesivir is a direct-acting antiviral drug, whereas baricitinib is an anti-inflammatory medicine.
The researchers found that patients on high oxygen by nasal canula or receiving breathing assistance with a mask when they were enrolled in the study had a time to recovery of 10 days with combination treatment versus 18 days with remdesivir and placebo.
Investigators also saw a difference in patient survival. The 28-day death rate was 5.1 percent in the combination therapy group and 7.8 percent in the remdesivir placebo group.
“We are making progress in the treatment of COVID-19,” said principal investigator Professor Thomas Patterson. “Remdesivir markedly improved recovery of critically ill patients in the first ACTT study and baricitinib further helped patients in this second study.”
Baricitinib is approved for the treatment of patients with active rheumatoid arthritis. The US Food and Drug Administration (FDA) issued an Emergency Use Authorisation (EUA) in November 2020, for baricitinib in combination with remdesivir for the treatment of suspected or laboratory-confirmed COVID-19 in hospitalised adults and paediatric patients two years of age or older requiring supplemental oxygen, invasive mechanical ventilation or extracorporeal membrane oxygenation.
“We do these clinical trials to accomplish a goal and that is to save lives,” Patterson said. “At the beginning of the pandemic, we were losing a lot of patients who we are now saving, so we are getting closer to our goal.”
The study was published in New England Journal of Medicine.
Related topics
Clinical Development, Clinical Trials, Research & Development (R&D), Therapeutics
Related organisations
University of Texas Health San Antonio, US Food and Drug Administration (FDA), US National Institute of Allergy and Infectious Diseases (NIAID), US National Institutes of Health (NIH)