Axi-cel highly effective in patients with advanced non-Hodgkin lymphoma, finds Phase II trial
Posted: 7 December 2020 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
Investigators report 76 percent of trial participants had a complete response to axicabtagene ciloleucel (axi-cel), despite being resistant to other therapies.
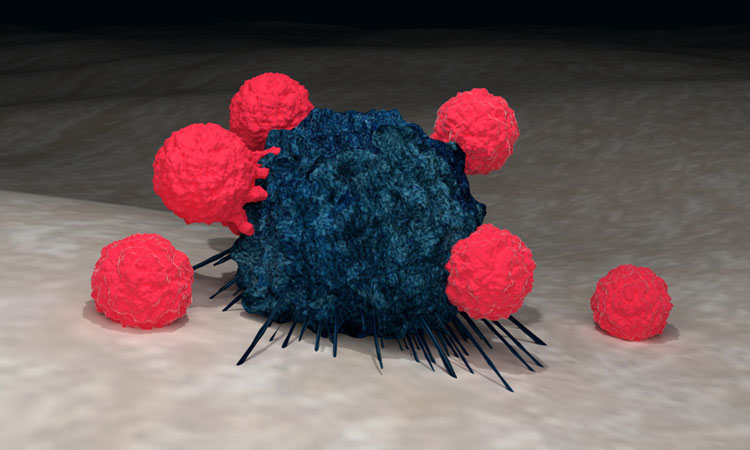
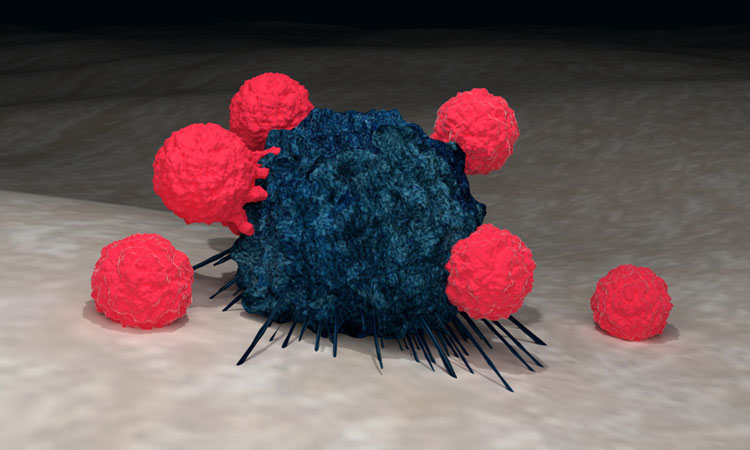
Axicabtagene ciloleucel (axi-cel), a chimeric antigen receptor (CAR) T-cell therapy, made cancer undetectable in more than three quarters of advanced non-Hodgkin lymphoma (NHL) patients treated in a Phase II trial.
According to Dana-Farber Cancer Institute investigators, despite the slow growth of NHL, patients often relapse after standard treatments, so there is a need to develop new therapies. The team said that the effectiveness of axi-cel in trial participants who had either relapsed or become resistant to other drugs is especially encouraging.
Axi-cel is made by collecting a patient’s T cells and genetically altering them to express a specialised, CAR receptor on their surface that allows them to target and destroy specific cancer cells. The CAR T cells are then infused into the patient. In previous trials in patients with large B cell lymphoma, the therapy reduced cancer cells below detectable levels – a complete response – in many patients.
In the current trial, called ZUMA-5, investigators administered axi-cel to 146 patients with follicular lymphoma or marginal zone lymphoma – two slow-growing forms of NHL – at multiple US medical centres. All had active lymphoma despite undergoing multiple previous treatments.
According to the investigators, after a median of 17.5 months after treatment, 92 percent of trial participants had a detectable reduction in their cancer cells (an objective response) and 76 percent had a complete response (cancer completely undetectable). At the cut-off date, 62 percent of patients were continuing to respond to axi-cel.
Almost all participants experienced adverse side effects, 86 percent had adverse events of grade 3 or higher. Seven percent experienced grade 3 or higher cytokine release syndrome and 19 percent experienced grade 3 or higher neurologic events. According to the investigators, patients with follicular lymphoma had slightly higher response rates and slightly less adverse effects than those with marginal zone lymphoma.
“We were very impressed with the magnitude of the responses and also the durability,” said Dana-Farber’s Dr Caron Jacobson, who led the trial and will present the findings at the virtual 62nd American Society of Hematology (ASH) Annual Meeting. “This treatment has meaningfully impacted high-risk patients with these diseases. I was also struck early on by how favourable the safety profile was compared to what we have been seeing in the fast-growing lymphomas.”