Novel formulation could provide solution to cancer vaccine shortcomings
Posted: 12 February 2020 | Victoria Rees (European Pharmaceutical Review) | No comments yet
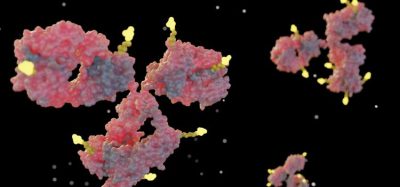
Researchers have developed a new formulation for cancer vaccines that could provide a solution to its delivery complications.


A team of researchers has developed a solution for the delivery challenges presented by cancer vaccines, using a new formulation.
First developed 100 years ago, vaccines for cancer have remained broadly ineffective. This is mostly due to tumour mutations unique to each patient, meaning that cancer cell antigens must be targeted extremely precisely, and a safe system is needed to deliver the vaccine to the intended location in order to induce a strong immune response.
The researchers from the Ecole Polytechnique Fédérale De Lausanne (EPFL), Switzerland, have now proposed a solution for this delivery problem. Using a polymerisation technique called polycondensation, they were able to develop a prototype vaccine which was successful in mice, that can travel automatically to the desired location and activate immune cells there.
The lead researcher Li Tang is also working with partners to develop an algorithm that can quickly and accurately predict mutated tumour antigens. Together, these two techniques should result in a new and better cancer vaccine in the next several years say the researchers.
How the vaccine works
The team explain how their vaccine will be effective; first, the patient is inoculated subcutaneously. The vaccine will then travel to the lymph nodes, where there are lots of immune cells. Once there, it is expected to penetrate dendritic cells. If the vaccine stimulates them correctly, the dendritic cells present specific antigens to cancer-fighting T cells, a process that activates and trains T cells to attack.
Using a polymerisation technique called polycondensation, they were able to develop a prototype vaccine”
However, as the components of the vaccine are very small, they tend to disperse or be absorbed in the blood stream before reaching the lymph nodes.
To overcome that obstacle, Tang and his team has developed a system that chemically binds the vaccine’s parts together to form a larger entity. The new vaccine, named Polycondensate Neoepitope (PNE), consists of peptide-based neoantigens and an adjuvant. When combined within a solvent, the components naturally bind together, forming an entity that is too large to be absorbed by blood vessels and that travels naturally to the lymph nodes.
Once inside a dendritic cell, the vaccine components separate again. This enables the dendritic cell to present the right antigens to the T cells, causing a powerful immune response. “This new vaccine, combined with a highly advanced analysis of each patient’s neoantigens, should allow cancer patients’ immune systems to be activated in a personalised and safe way,” said Tang.
The team is still perfecting the stage at which the tumour-specific antigens are detected. “This identification stage is just as vital,” concluded Tang. “Since these neoantigens aren’t present in healthy cells, accurate identification will allow us to target tumour cells very precisely, without any toxicity in healthy tissue.”
The study was published in ACS Central Science.
Related topics
Formulation, Preclinical Research, Research & Development (R&D), Therapeutics, Vaccine Technology, Vaccines