Personalised medicine, batch size of ONE, the new challenge to fill-finish?
Posted: 29 June 2017 | Wenzel Novak PhD | Market Development Director – Pharma | Optima Machinery Corporation | No comments yet
Wenzel Novak PhD gives some considerations on container, environment, process and automation for small batch sizes in the downstream process of fill-finish…


The market for new biopharmaceutical drugs was investigated by the Boston Consulting Group in its study “R&D Productivity 2014: A Breakthrough Year for Biopharma.” 2014 was a record year in terms of approvals by the FDA: 53 new therapeutic drugs (NTDs) were approved. Conservative estimates of revenues from these drugs in 2014 are $48 billion, a figure significantly above the 25-year average of $36 billion. The numbers are even more impressive when compared to research spending. Total R&D expenditures in the industry have remained relatively constant since 2008 at $140 billion, including in 2014. Boston Consulting considers this on average an acceptable relationship between research expenditures and revenues for NTDs, an important prerequisite for sustainable and ongoing investment.1
Personalised medicine
Personalised medicine describes a wide area of individualised applications, with one point in common. The need to handle a small number of containers, often suitable only for one patient. From a fill-finish perspective, we can name some candidates for small batch sizes.
It can be a disease with only very restricted potential patients. FDA defines orphan disease as a condition that affects fewer than 200,000 people nationwide, but can be even less than one hundred.2
It might be new monoclonal antibodies (NMEs) based on individual biomarkers, suitable only for a restrict number of patients. In the last three years more than 20% of NMEs approved by CDER can be put into this category.3
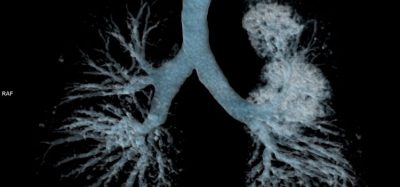
The EMA (European Medicines Agency) classifies therapies based on substantially manipulation of cells, not intended to be used for the same essential function as ATMPs (Advanced Therapy Medicinal Products).4 In the US, the phrase “cell and gene therapy” is more typically used. The basic approach of gene therapy is replacing a mutated gene that causes a disease with a healthy copy. Thereby inactivating, or “knocking out,” a mutated gene that is functioning improperly or introducing a new gene into the body to help fight a disease.5 Cell therapy is defined as the administration of live whole cells or maturation of a specific cell population in a patient for the treatment of a disease. Expression from specific molecules might affect a broad range of diseases or used for eliminating specific cancer cell.6
Currently we see a split between autologous and allogenic efforts. Even if we follow the allogenic path, we will make only a quite low number of treatments on an individual patient (based on the idea: “it’s a cure not a lifelong treatment”). Autologous means donor and patient are the same. So we will face a sophisticated logistic and even a much lower applications “one drug – one patient”.
Personalised medicine or even cellular therapies are not a new concept. In 1907, Reuben Ottenberg reports the first known blood compatibility test for transfusion using blood typing techniques and cross-matching between donors and patients to prevent hemolytic transfusion reactions.
But rapid developments in genomics, together with advances in a number of other areas, such as computational biology, medical imaging, and regenerative medicine, are creating the possibility for scientists to develop tools to truly personalise diagnosis and treatment.7 In consequence, the “one size fits all” treatment might become less relevant in the following decades. In the end, we will have to take care of a fragile living organism (cell), with restriction to storage conditions, a limited acceptance to shear forces and a high requirement of an appropriate treatment over all.
Downstream processes
Downstream processes are most often not in the focus of R&D groups. However, fill-finish will be a focus of production, quality and regulatory. Next to all the challenges in apheresis, R&D, manufacturing, storage and logistics, we have to choose the proper container, filling a pharmaceutical and close it, for human use. Not to forget we are required to fulfil the common rules of aseptic processing and to follow cGMP guidance in a commercial process.
Fill-finish is mainly, but not in total, related to the chosen container, the adequate filling and closing itself, the added controls and checks, the (possible) grade of automation and the environment we work in.
Containers
In many cases, the typical container for distribution in the “classic big pharma business” is made of glass. Most time it’s a vial or a syringe. Just think about, how often we finally have to apply the liquid medication by a syringe to the patient. However long-term storage, added procedures just before application or multi-use approaches may indicate for a different storage container. Polymers as PP are often used for the final application but most of the time are not suitable for product storage over a longer period. To choose the best material we have to consider several aspects like breakability (rough environment e.g. ambulance), permeability of gasses (oxygen sensitive products), leachables and extractables (container interference with the product), adhesion properties (cell and protein), coating as silicone on the inside or silicone free systems (silicone may effect product-characteristics, aggregation and application forces) and the storability (e.g. in liquid Nitrogen and correlated effects on container closure integrity).
Glass
Glass is a well-characterised material for primary packaging containers. It has a quite good number of excellent features such as permeability; it has its restrictions in the contact with cells and proteins (relatively high adhesion forces lead to a product loss due to sticking on the surface). Siliconisation might minimise loss of product due to adhesion but can initiate aggregation on the other hand. Not to forget living cells might be frozen in the liquid phase of Nitrogen. The chosen container and closure has to accept the temperature of below 77K without significant breakability and sterility issues. Importantly, the container closure integrity needs to work at this temperature. Reliable studies are often missing that aspect, in contrast to studies showing potential cross contamination in the liquid phase.
Polymers
Polymer containers are available in a wide variation today. High quality containers for long-term storage are typically made of Cyclic Olefin Copolymer (COC) / Cyclic Olefin Polymer (COP). This material shows a high break resistance, low permeability (compared to other polymers) and minimal leachable and extractable profiles. COC/COP accepts low temperatures and is clear (suitable for visual inspection). It’s already been used for more than a decade in the pharmaceutical industry in significant numbers and has proven to be of reliable quality. Remembering the high protein glass adhesion, polymers offer an excellent alternative as primary packaging material, if it is required.
Type of container
Bags are still often used for storage of cell suspensions and in the blood business. But bags are not common for classical pharmaceutical products. Maybe the traditional hospital-approach for apheresis is to go with a bag; and then maybe a lot of development teams just stay with it. It allows easy mixing, can be frozen and the storage logistic is established (blood banks). Permeability for decontamination detergences as Hydrogen-Peroxide is clearly questionable. Avoiding damage (pin holes) and inspection on a bag is a hard job. Not to forget, the residual volume might be above the tolerable volume. Keeping in mind an automated process, bag flexibility does not make the job easier. As long as we deal with higher volumes in the process, bags are a reasonable solution. However, getting into the small volume and small batch fill-finish processes it complicates automation and adds some back draws to the process stability.
Glass and polymer vials are available in all sizes and offered by several suppliers in an already pre-cleaned and pre-sterilised design. All downstream and logistic aspects are well tried. One concern however is closure integrity at low temperatures. We typically have a system of vial, stopper and cap; for perfect functionality all the components have to work together. A special concept, named “close vials” melts the polymer vial together with the cap. Filling is now done with a needle through the elastomeric inlay of the cap. A laser seals the puncture after filling.
As already discussed, the product needs to be extracted out of the vial manually using a syringe. The residual volume is correlated to container hydrophobicity and the capabilities of the health employee applying the product to the patient, but never even close to zero.
Glass and polymer syringes
Glass and polymer syringes allow a direct fill into the final application device (single dose). Therefore, the dead volume will be the lowest achievable for application. Needed overfill is reduced to a minimum. It eliminates a significant part of handling steps that are out of control by the manufacture. If needed, silicone free systems are on the market. Be aware no washing steps (reduce e.g. DMSO) can be implemented easily and to reiterate, container closure integrity at low temperatures has to be validated.
Special designed cartridges can offer a mixture of features needed for the specific product. One of these systems allows direct connection to the typical tubing sets in a hospital, adds the capability to get the product directly into a syringe and even offers a tube connection for sampling.
One system is still missing. A closed system, sometimes named “from needle to needle” would be a perfect solution. We do not need to care about sterility issues and highly controlled environment. Nevertheless, it takes away flexibility in volume, process design and comes with a high complex system to handle along the process. A weak point today is the availability of suitable sterile interfaces. Connecting and disconnecting different containers during the complete process without jeopardising the inside sterility is not established yet perfectly and in conformation to regulations.
Fill-Finish
Fill-Finish describes the core process of filling and closing the primary container. Filling will be often done by a peristaltic pump or even manually using a syringe. A peristaltic pump allows the creation of a (nearly) closed, disposable filling system with high flexibility in the setup. Processing high viscose products or very small filling volumes; alternatives such as rotary piston pumps and others might be the preferred option. Often only intense customer – supplier discussions and filling tests will get to the best filling pump system. Cells are shear force sensitive, this aspect has to be considered while discussing the filling system, filling speed and testing. Just do not forget; a typical needle for final application and a high application rate will add significant shear forces. Pro and cons of each systems needs to be evaluated individually for each product. But seeing the advances of disposable filling paths and the fantastic flexibility on filling, a peristaltic pump will be a good starting system to think about.
The method and type of closure depends mainly of the chosen container. Bags are often just connected with a tube and welding is the preferred method. Vials will go with an elastomer stopper and a crimped cap with it. Instead of aluminum caps, snap on plastic caps are offered too, just still in a kind of pre-market stage. Syringes will be stoppered in line with an elastomeric plunger, sometimes coated to improve functionality. Different processes will require specific equipment. Most available systems will offer the capability to handle one type of container to be used on a fill-finish “line”. Only newer concepts allow the handling of several types of container on one filling machine; even without manual intervention to change the set-up. Strict manual handling is most often used only with bags. Vials, syringes and cartridges need at least a supporting device to close the container.
Control / check
Any process step influencing the product quality or the sterility has to be controlled based on qualification data. Manual handling such as sealing can often not be qualified (time, pressure, temperature, data recording) so an even more intensive checking of the result is needed. A risk analyses should cover the patient relevant risk at least. This will be all product-affecting deviations, including potential sterility issues and not to forget about the consequences for the patient in case of total product loss. Often not considered are the economic risks. You cannot compromise on patient safety, but economic risk, such as a clinical trial failure, loss of product or increased quality assurance procedures or production costs can be set in the right context to find the best balance between costs and risk. These considerations will make the decision on the (automatic) controls and checks to be add to the process. Just imagine the advantages of a parametric release at the end of a manufacturing process without the need of intensive testing and wasting of product.
Automation
One option to achieve a reproducible process is it to avoid variations by the operator. Although we often deal with variations in the primary material (patient correlated), any further process variations will increase the insecurity of the final product quality and the therapy result. However, automation will ask for strictly fixed processes and for containers and interfaces, which are well defined. It takes away the flexibility common standard in R&D driven companies. Commercialisation is demanding on reproducible processes, following rules and not about the operators’ performance today. Supplier and users have to create solutions, which gain the needed flexibility but are restrictive enough to guarantee a known outcome on product quality. Finding these perfect spots will be the challenge that we have to take in the next years.
Environment
Aseptic processing in ISO 5 (ISO 14644-1) / class A (100) is must. Working in a low turbulent air flow cabinet is good common practice (often consistent first air contact on the open product is a challenge). We see masked and nicely gowned operators working in laminar workbenches based on a traditional zone concept. Even if it is a well-accepted standard, we create gowning costs (often underestimated), an uncomfortable working situation and we need a lot of trust to our well-trained operators for proper handling.
Nevertheless, we lower investment costs and gain flexibility compared to Isolator concepts (fully closed aseptic area). Not often considered is the TCO (total cost of ownership) involving the daily costs, a typical calculation shows an ROI (return of investment) for Isolator based technologies in 3 years. Even more important, using Laminar-flow-workbenches and manual sterilization methods we have to accept an increased sterility and process risk, due to the direct interference of product and operator. Training of operators and well-established quality assurance procedures are key to stay safe. To jeopardise the efforts of years’ of work and millions in investment due to a bad day in the operators life is a nightmare we likely do not want to face.
Putting all critical steps into a closed environment will reduce significantly the operators influence on the product quality and minimise non-sterility risks. Although it takes away some comfort by handling process steps inside an Isolator through gloves, it allows for exactly the same handling as used in a laminar-flow-workbench. Since an Isolator is placed in an ISO 7/8 (C/D) area, no relevant restrictive gowning will be required for the operators. The inside of such an isolator is decontaminated by Hydrogen-Peroxide and sometimes even washed or whipped automatically. These processes are highly reproducible and can be validated during the qualification phase. Although separation between operator and product (sterility) is the main focus on an Isolator based production, the restrictive access adds significant reproducibility to the complete process flow by itself. It is basic to guarantee a controlled and checkable operation. Any interaction of operator and product can be recorded. Process deviations are much less likely.
Conclusion
There is a fundamental difference between producing blockbuster drugs and small batches of niche products, as it is typical for biopharmaceuticals. Of significant importance in this scenario are the filling and packaging processes, which also play an important role in successful flexibilisation strategies. For clinical phases, in highly manually based processes, automation may be introduced with operator guidance through the process and allow a tight process check on all relevant parameters. When visualising commercial production, that would be the latest moment to consider minimising process and sterility risks and also reducing the cost of production. An isolated controlled environment, a fill-finish process based on a standard container and a highly automated system is, I believe, the solution to go for. Take the experience from traditional “big pharma” production and adapt it for the future. Automated fill-finish processing a one-container batch can be as safe and reproducible as any established process for a 1-Million vaccine batch.
Aseptic processing training
The PDA is running a two-day training course on ‘Best Practices and Points to Consider in Aseptic Processing’ to be held on November 9-10 in Vienna, Austria. The course aims to facilitate a deeper understanding and provide insights into the aseptic processing environment, and to go beyond what is commonly covered in books on the subject. A practical and highly interactive approach will enable participants to get actively involved, discussing guidelines and warning letters, in addition to sharing perspectives and solutions to issues found in everyday job situations. For more information, visit: www.pda.org.
Biography
After studying biology, Dr Wenzel Novak did his PhD in physics at the Max-Planck-Institute for Neurochemistry in Munich.
His first role was head of a laboratory in a biotech-company based in Germany and Switzerland. The main interests of this company was differentiation and cultivation of skin-sheets, created out of hair roots (Keratinocytes) used for wound healing.
As head of production for presterilsed containers, in a company manufacturing plastic and glass primary packaging components, he designed and built the manufacturing area, installed the QA-system and operated the start-up phase of production.
He spent 10 years with a supplier of pharmaceutical equipment and served on the managing board as Chief Research Officer. Central to his business was to improve the knowledge base of standard processes and looking into new attempts to be used in filling and attendant pharmaceutical processes.
Since 2016, he holds position as Market Development Director in an international technology company, focusing on fill-finish processes, environmental control and packaging. His main focus is the market based development of equipment for new therapies and processes.
References
(1) https://www.bcg.com/en-us/default.aspx
(2) https://www.fda.gov/Drugs/ResourcesForYou/Consumers/ucm143563.htm
(3) http://www.personalisedmedicinecoalition.org/Userfiles/PMC-Corporate/file/PM-at-FDA.pdf
(5) https://ghr.nlm.nih.gov/primer/therapy/genetherapy
(6) http://www.asgct.org/general-public/educational-resources/gene-therapy–and-cell-therapy-defined
(7) https://www.fda.gov/downloads/scienceresearch/specialtopics/personalisedmedicine/ucm372421.pdf
Related topics
Antibodies, Big Pharma, Biomarkers, Biopharmaceuticals, Financial Results, Gene therapy, Imaging, Packaging, Personalised medicine, polymers, Research & Development (R&D), Single Use
Related organisations
European Medicines Agency (EMA), U.S. Food and Drug Administration (FDA)