Neurotoxicity in preclinical studies
Posted: 3 December 2008 | David E. Ray, Associate Professor of Neurotoxicology, School of Biomedical Sciences, University of Nottingham, United Kingdom | No comments yet
Neurotoxicology is not a discipline that can expect to be popular in pharmaceutical circles. It is a not unreasonable prejudice amongst people working in drug development that even a suggestion that a candidate drug might be neurotoxic is enough to halt development, or at the least to stimulate a highly motivated search for an alternative. There are several good reasons for this. Firstly, neurotoxicity can be highly disabling and irreversible. Secondly, it is hard to detect (or rather to exclude) via high throughput systems. Thirdly, it is often hard to understand.
Neurotoxicology is not a discipline that can expect to be popular in pharmaceutical circles. It is a not unreasonable prejudice amongst people working in drug development that even a suggestion that a candidate drug might be neurotoxic is enough to halt development, or at the least to stimulate a highly motivated search for an alternative. There are several good reasons for this. Firstly, neurotoxicity can be highly disabling and irreversible. Secondly, it is hard to detect (or rather to exclude) via high throughput systems. Thirdly, it is often hard to understand.
Neurotoxicology is not a discipline that can expect to be popular in pharmaceutical circles. It is a not unreasonable prejudice amongst people working in drug development that even a suggestion that a candidate drug might be neurotoxic is enough to halt development, or at the least to stimulate a highly motivated search for an alternative. There are several good reasons for this. Firstly, neurotoxicity can be highly disabling and irreversible. Secondly, it is hard to detect (or rather to exclude) via high throughput systems. Thirdly, it is often hard to understand.
However, there are also good reasons not to over-react. Most neuro-active drugs have the potential to produce overdose neurotoxicity, and yet have made it successfully into the market. There is also a good pool of knowledge about neurotoxicity that can be drawn on by anyone in the industry who is unfortunate enough to need it. At this point, as past-President, I would like to briefly mention the International Neurotoxicology Association (INA). This is a non-profit making organisation with approximately 120 members world-wide who are dedicated to improving the academic discipline of neurotoxicology. Details of INA and its biennial scientific meetings can be found on the web at http://www.neurotoxicology.org. I would strongly recommend anyone who needs further information to contact INA, since its membership includes experimental scientists, physicians, and regulators – all with a wide range of expertise in the area. Whilst INA members may not be able to provide answers, they should be able to provide useful advice and put questions into a broader context. There are also a number of excellent (if sometimes intimidatingly thick) books that cover the topic of neurotoxicology. A very comprehensive description of most specific neurotoxicants and of general principles is given by Spencer et al.1, while clinical aspects are covered by Feldman2, and methodology by Chang and Slikker3.
To return to the reasons for disliking neurotoxicity, the most obvious one is the nature and severity of the disability that can be produced. The brain is somewhat unusual in having very little reserve capacity. Thus loss of a lung, kidney, or liver lobe can be compensated for very effectively, whereas loss of even a small brain area, as in a stroke, can be massively disabling. Within the central nervous system, nerve cells are terminally differentiated, and cannot replace themselves. The potential for replacement by endogenous stem cells is limited to a few specific regions such as the hippocampus, and usually even the re-growth of damaged nerve fibres in the brain or spinal cord is blocked. This poor repair capacity means that even if the neurone survives but the nerve fibre is lost, life-long disability can result. This happened with the spastic paralysis caused by some organophosphorus esters (fortunately a small minority of them), where many people have developed a severe disability as the result of just a single exposure4. In addition, most kinds of brain dysfunction have a greater impact in terms of socio-economic attainment than do equivalent liver or lung dysfunctions. This means that neurological disorders have a disproportionate cost in terms both of lost human potential and care needs5. So the stakes are high: there is a lot to be gained by treating neurological disorders with safe and effective drugs, but there is also a lot that could be lost by any unexpected neurotoxicity. There are several examples of such neurotoxicity produced by pharmaceuticals: fortunately mostly from the era when neurotoxicology was in its infancy. A remarkable instance was that of Stalinon, which was marketed by a French pharmacist in the 1950s for treatment of skin infections (see Figure 1).
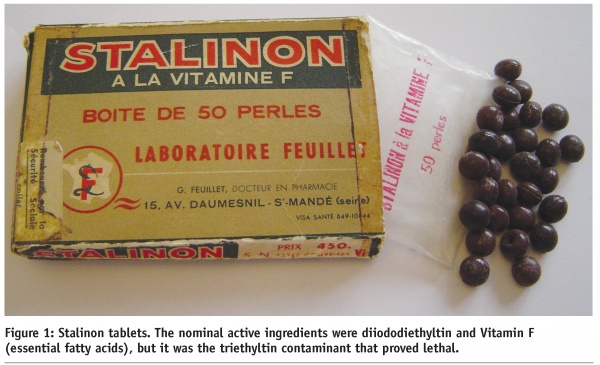
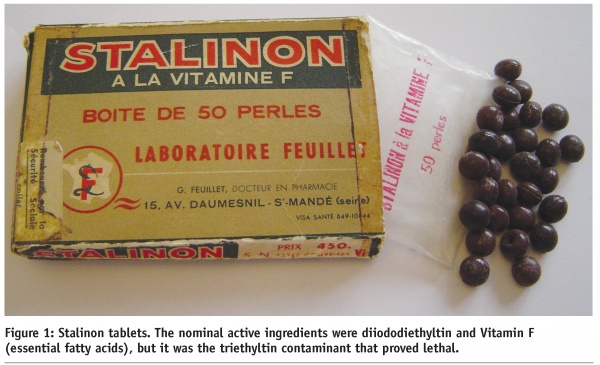
Stalinon was contaminated during manufacture by approximately 10% of triethyltin, and this untested constituent resulted in 102 deaths and many cases of disability in patients who had taken Stalinon. This reflected the very specific potential of triethytin to reach and damage brain and spinal cord myelin6; an effect that would in fact have been easy to detect in simple animal models had the formulation (rather than the active) been tested. Another example of a neurotoxic pharmaceutical is the anti-epileptic valproate. The teratogenic potential of valproate was recognised as a result of animal studies7, but not in time to prevent human cases of spina bifida. Indeed valproate and other anti-epileptic drugs can still present physicians with difficult choices, since it may be the only drug that controls seizures in a pregnant patient but, if taken at a dose sufficient to ensure a seizure-free pregnancy, it may also impair brain development and reduce intelligence in the child8. Fortunately the anti-epileptic and the teratogenic effects of valproate are mediated by actions at different molecular targets9, and so it should prove possible to eliminate this neurotoxicity in the next generation of drugs.
The developmental effects of valproate on intelligence are probably irreversible, and this highlights developmental neurotoxicity, which is often irreversible, and hence a particular cause for concern. Development and maturation of neuronal circuits within the brain occurs not only as a result of pre-programmed development, but also (in its later stages) as a result of functional interactions resulting from sensory and motor experience. These interactions are susceptible to pharmacological influences, and it has been recognised for some time that if the brain matures under the influence of a neuroactive drug, it may develop abnormally. The developing brain can also lack the capacity that is present in the adult brain of returning receptor expression and neurotransmitter release to normal after drug exposure has ceased. An early example of this was provided by the lasting effects of pre- or post-natal exposure to haloperidol in rats10. The effects of perinatal diazepam are also very long lasting in rats11. Hopefully such effects are not seen at the doses used in man, but the use of any form of neuroactive drug during pregnancy, and particularly in young children needs to be very cautious. This need for caution is well illustrated by elemental lead. Its potential to produce developmental neurotoxicity has been known for many years, and now its mechanism of action on the NMDA receptor is also quite well understood12. However, this has not made it a simple matter to determine a tolerable exposure level for lead, since its effects lack a very clear threshold, and merge into factors such as how stimulating the child’s environment and education are. A consequence of this is that the internationally recognised threshold levels for blood lead in children have been gradually reduced from 60 μg/dl in the 1960’s to 10 μg/dl at present as more epidemiological evidence of relatively subtle but lasting adverse effects has accumulated. Similar considerations will apply to pharmaceuticals, where the potential for toxicity has to be carefully balanced against the therapeutic benefit, rather than (as with lead) the cost of environmental decontamination.
Difficulty of prediction of neurotoxicity is illustrated by tardive dyskinesia, a slowly developing condition involving involuntary movements that is produced by a number of antipsychotics, including chlorpromazine. The exact causes of this important drug side-effect are not well understood and, although it does slowly resolve after treatment is stopped, it can be disabling. It was originally thought that the newer generation of drugs had little potential to cause tardive dyskinesias, but experience has indicated that, although early drug trials were encouraging, with longer durations of treatment the incidence is not much lower than with the older antipsychotics13. Slowly developing neurotoxicity can be very difficult to predict in animal models or in vitro unless the mechanism is understood, which evokes the second problem mentioned at the beginning of this article, that neurotoxicity is hard to detect or exclude.
Neurotoxicity is hard to detect because it can take many different forms. An outline of these are given in Box 1.
These examples show that neurotoxicity is not simply a matter of cytotoxicity, or even of lesser forms of morphological damage. Lethal neurotoxicity can result from purely functional disruption, dramatic examples being the direct excitation produced by the pyrethroid insecticides, which act by prolongation of sodium channel open time14, or the indirect excitation seen following loss of spinal cord and brainstem inhibition produced by the glycine antagonist strychnine. In neither case are their lethal effects accompanied by anything other than secondary morphological damage, and they have very little capacity to produce cytotoxicity in vitro. Where neurotoxicity is associated with morphological damage it is very often restricted to a sub-population of cells in a specific set of brain areas. The cell type and the brain area involved vary greatly with the chemical nature of the drug or chemical, although some regions are more vulnerable than others to a range of agents. Furthermore, very few of the substances that produce neuropathological damage target more than approximately 10% of the brain at survivable dose levels. This can mean that a superficial examination of the brain may miss localised damage. A very clear example of this localised damage is provided by trimethyltin, see Figure 2, an industrial chemical that has also poisoned humans. The acute signs of toxicity are very obvious (in man: acute paranoia, seizures), but the damage is (in the rat, and probably in man) localised to specific sub-areas of the limbic system.


Fortunately it is possible to use various histological methods to highlight and to quantify these damaged areas within the brain, most notably silver degeneration stains15, and modern immunohistochemical methods that visualise the changes in gene expression of astrocytes and microglia that occur within 2-3 days of even a minor degree of morphological damage. Morphological methods are not necessarily restricted to post mortem use, and MRI imaging has proved to be a good method of detecting localised neurotoxicity, as illustrated by the brainstem lesions produced by the male contraceptive, 3-chloropropanediol. These lesions were clear even in animals that showed no obvious change in behaviour, and quantification of serial MRI scans indicated that only approximately 9% of the brain was susceptible to damage16.
Such focal morphological lesions are relatively easy to detect if the brain is properly examined using modern methods, and is free from post-mortem artefact. However diffuse morphological changes, such as decreased synaptic density, or purely functional damage are more difficult to detect. Neurobehavioural tests have proved useful in man17, and both simple observational18 and more sophisticated tests19 have been developed for use in animals. It can however be far from simple or convenient to use these neurobehavoural methods to screen for potential neurotoxicity in candidate pharmaceuticals. Because different aspects of behaviour are changed by different neurotoxicants, no single measure is sufficient to screen for an effect, or to establish an acceptable negative. This means that multiple tests must be used, and this is both expensive (to test one chemical in one species will cost at least €500K); and also difficult to interpret, since multiple end points, often with high coefficients of variation, are involved20.
However, developmental neurotoxicity represents the most difficult manifestation of neurotoxicology, and effects in the adult are often much easier to detect. Neurotoxicity in adult animals usually shows up as a change in behaviour, careful observation of which often gives clues as to the location of the functional system involved. There are no known human neurotoxicants that cannot be detected using appropriate animal models – although specific manifestations of toxicity and dose thresholds may vary. Thus the human polyneuropathy caused by exposure to some organophosphorus esters mentioned earlier is detectable by motor signs in hens and most large mammals, although it produces only morphological changes in rodents.
Animal based methods are however not very practical, cost-effective, or humane in the context of high-throughput screening, and this brings us to the final difficulty: neurotoxicity is difficult to understand. The fundamental reason for this is simple. Although therapeutic drugs are intended to fulfil one well-defined purpose, toxic chemicals are free to disrupt any biological system that they can reach. The question “is it safe” is always going to be more difficult to answer than “does it work”. The potential of a candidate pharmaceutical to produce neurotoxicity cannot be circumscribed to fall within a pre-defined set of target systems or mechanisms of action. Knowledge of the mechanism of efficacy of a candidate drug can be very helpful, but neurotoxicity has been seen from agents that were never designed to act on the nervous system – most obviously antibiotics. In fact most of the toxic chemicals that I have worked on have turned out to act on or via molecular targets that would otherwise be left in decent obscurity, and would not be likely to form part of a prospective pharmaceutical screening battery. This list includes calcium-insensitive voltage-gated chloride channels14, brain nitroreductase21, an intracellular phospholipase22, and other as yet undefined targets.
However neurotoxicologists are making advances in the understanding of mechanisms, and a number of neurotoxicants are now recognised to fall into classes (such as receptor agonist neurotoxicants) that enable structure-activity relationships to be defined. This is in part a response to the needs of the pharmaceutical industry and also the demands of regulators to assess the thousands of natural and man-made chemicals that have not been given a neurotoxicological evaluation. After rather a long fallow period, in vitro neurotoxicologists have also recognised that neurotoxicology is not restricted to cytotoxicity, and that functional assays need also be incorporated into their screening systems23. Even in the area of developmental neurotoxicity neurotoxicologists are evaluating the potential for medium through-put screens24 – although it will be difficult to include sufficient of the features that determine vulnerability to be able to establish a convincing negative in this most challenging of areas.
In summary, neurotoxicity is indeed bad news, but it can often either be avoided or banished to the high overdose realm if a sufficiently intelligent approach is taken to understanding it.
References
- P.S. Spencer, H.H. Schaumburg, and A.C. Ludolph, Experimental and clinical neurotoxicology, Oxford University Press, New York, Oxford, 2000.
- R.G. Feldman, Occupational and environmental neurotoxicology, Lippincott-Raven, Philadelphia, 1999.
- L.W. Chang and W. Slikker, Neurotoxicology: approaches and methods, Academic Press, San Diego, 1995.
- M. Lotti and A.Moretto, Organophosphate-induced delayed polyneuropathy, Toxicol. Rev. 24 (2005) 37-49.
- M. Sillanpaa, P.ndlin-Sobocki, and J.Lonnqvist, Costs of brain disorders in Finland, Acta Neurol. Scand. 117 (2008) 167-172.
- J.M. Barnes and H.B.Stoner, The toxicology of tin compounds, Pharmacol. Rev. 11 (1959) 211-231.
- N.A. Brown, J.Kao, and S.Fabro, Teratogenic potential of valproic acid, Lancet 1 (1980) 660-661.
- T. Tomson and D.Battino, Teratogenic effects of antiepileptic drugs, Seizure. 17 (2008) 166-171.
- N. Gurvich, M.G.Berman, B.S.Wittner, R.C.Gentleman, P.S.Klein, and J.B.Green, Association of valproate-induced teratogenesis with histone deacetylase inhibition in vivo, FASEB J 19 (2005) 1166-1168.
- H. Rosengarten and A.J.Friedhoff, Enduring changes in dopamine receptor cells of pups from drug administration to pregnant and nursing rats, Science 203 (1979) 1133-1135.
- Y.H. Raol, G.Zhang, E.C.Budreck, and A.R.Brooks-Kayal, Long-term effects of diazepam and phenobarbital treatment during development on GABA receptors, transporters and glutamic acid decarboxylase, Neuroscience 132 (2005) 399-407.
- C.D. Toscano and T.R.Guilarte, Lead neurotoxicity: from exposure to molecular effects, Brain Res. Brain Res. Rev. 49 (2005) 529-554.
- C.U. Correll and E.M.Schenk, Tardive dyskinesia and new antipsychotics, Curr. Opin. Psychiatry 21 (2008) 151-156.
- D.E. Ray and J.R.Fry, A reassessment of the neurotoxicity of pyrethroid insecticides, Pharmacol. Ther. 111 (2006) 174-193.
- A.S. Fix, S.R.Stitzel, G.M.Ridder, and R.C.Switzer, MK-801 neurotoxicity in cupric silver-stained sections: lesion reconstruction by 3-dimensional computer image analysis, Toxicol. Pathol. 28 (2000) 84-90.
- M.J.W. Prior, A.M.Brown, G.Mavroudis, T.Lister, and D.E.Ray, MRI characterisation of a novel rat model of focal astrocyte loss, Magnetic Resonance Materials in Physics Biology and Medicine 17 (2004) 125-132.
- G. Winneke, Appraisal of neurobehavioral methods in environmental health research: the developing brain as a target for neurotoxic chemicals, Int. J. Hyg. Environ. Health 210 (2007) 601-609.
- V.C. Moser, The functional observational battery in adult and developing rats, Neurotoxicology 21 (2000) 989-996.
- T. Sagvolden, V.A.Russell, H.Aase, E.B.Johansen, and M.Farshbaf, Rodent models of attention-deficit/hyperactivity disorder, Biol. Psychiatry 57 (2005) 1239-1247.
- R.R. Holson, L.Freshwater, J.P.Maurissen, V.C.Moser, and W.Phang, Statistical issues and techniques appropriate for developmental neurotoxicity testing A report from the ILSI Research Foundation/Risk Science Institute expert working group on neurodevelopmental endpoints, Neurotoxicol. Teratol. 30 (2008) 326-348.
- H.L. Hu, N.Bennett, J.H.Lamb, J.F.GhersiEgea, B.Schlosshauer, and D.E.Ray, Capacity of rat brain to metabolize m-dinitrobenzene: an in vitro study, Neurotoxicol. 18 (1997) 363-370.
- O. Zaccheo, D.Dinsdale, P.A.Meacock, and P.Glynn, Neuropathy target esterase and its yeast homologue degrade phosphatidylcholine to glycerophosphocholine in living cells, J Biol. Chem. 279 (2004) 24024-24033.
- A.K. Bal-Price, C.Sunol, D.G.Weiss, V.E.van, R.H.Westerink, and L.G.Costa, Application of in vitro neurotoxicity testing for regulatory purposes: Symposium III summary and research needs, Neurotoxicology 29 (2008) 520-531.
- S. Coecke, A.M.Goldberg, S.Allen, L.Buzanska, G.Calamandrei, K.Crofton, L.Hareng, T.Hartung, H.Knaut, P.Honegger, M.Jacobs, P.Lein, A.Li, W.Mundy, D.Owen, S.Schneider, E.Silbergeld, T.Reum, T.Trnovec, F.Monnet-Tschudi, and A.Bal-Price, Workgroup report: incorporating in vitro alternative methods for developmental neurotoxicity into international hazard and risk assessment strategies, Environ. Health Perspect. 115 (2007) 924-931.
Box 1
Some of the very different manifestations of neurotoxicity (with examples and outline mechanisms)
Pharmacological neurotoxicity:
- Simple overdose (barbiturates: respiratory failure)
- Acute Reactive (triazolam: rebound agitation on drug withdrawal)
- Chronic Reactive (chlorpromazine: D2 receptor upregulation, dopamine hypersensitivity, tardive dyskinesia)
- Developmental (haloperidol: perinatal exposure changes receptor profile)
Morphological neurotoxicity:
- Direct (adriamycin: dorsal root ganglion cell and cochlear hair cell death)
- Indirect (chronic ethanol: thiamine lack causing glial death and then neuronal loss)
- Developmental (lead: paucity of synapse formation via NMDA receptor effects)




