Regular infusions of a novel antibody may suppress HIV for four months
Posted: 18 April 2019 | European Pharmaceutical Review | No comments yet
According to a new report, regular infusions of an antibody that blocks the HIV binding site on human immune cells may have suppressed levels of HIV for up to four months in people undergoing a short-term pause in their antiretroviral therapy (ART) regimens.
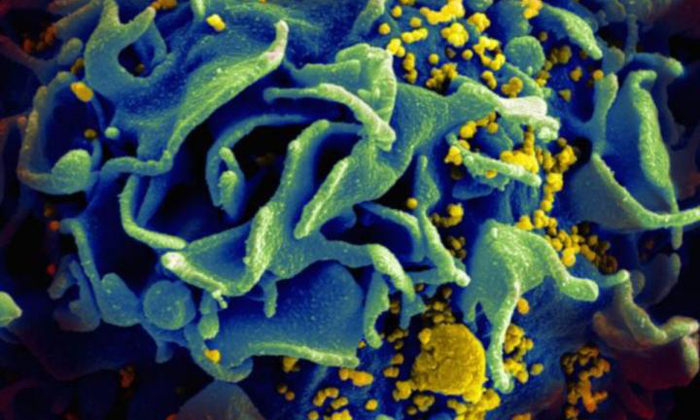
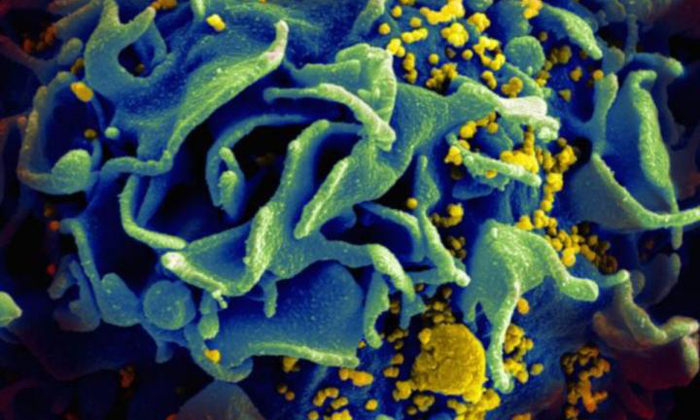
Microscopic image of an HIV-infected T cell (credit: NIAID)
Results of the phase II, open-label study indicate the antibody, known as UB-421, was safe and did not induce the production of antibody-resistant HIV.
The study, which was conducted in Taiwan and led by Chang Yi Wang, PhD, Chief Scientific Officer and Chairperson of United BioPharma, Inc, had 29 volunteers with well-controlled HIV discontinue their normal regimens of daily oral ART at the time of their first infusion or one week later, depending on their ART regimen.
In total, 14 participants received eight regular weekly infusions of UB-421, while 15 received eight higher-dose infusions every other week. At the end of the eight- or 16-week treatment period, all volunteers restarted their previous ART regimen and were evaluated in follow-up visits up to eight weeks later.
Apart from a single participant who discontinued the study due to a mild skin rash, volunteers in both groups maintained HIV suppression (plasma HIV RNA levels under 20 copies/mL) throughout the treatment period in the absence of ART.
Previous experimental infusions of broadly neutralising antibodies, or bNAbs, have suppressed HIV for around two weeks by targeting proteins on the virus itself, but the rapid mutation rate of HIV induces antibody-resistant strains that render the treatment ineffective. UB-421 theoretically avoids this possibility by blocking a stable human protein that HIV uses to infect T cells. Indeed, resistance to UB-421 was not seen at all in this study.
The report was published in The New England Journal of Medicine. Further studies have been planned in Taiwan and Thailand to evaluate the safety and efficacy of UB-421 as a treatment for HIV.
Related topics
Analytical techniques, Antibodies, Clinical Trials, Research & Development (R&D), t-cells