Arthritis drug baricitinib re-aimed to target diabetic kidney disease
Posted: 10 June 2015 | European Pharmaceutical Review
Researchers have presented promising results from a clinical trial of the experimental drug baricitinib in people with diabetic kidney disease…
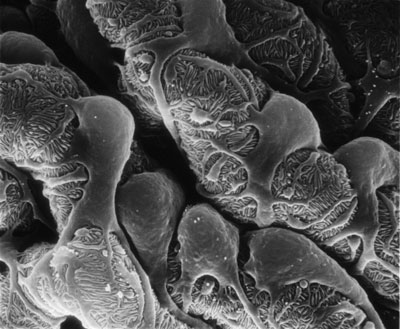
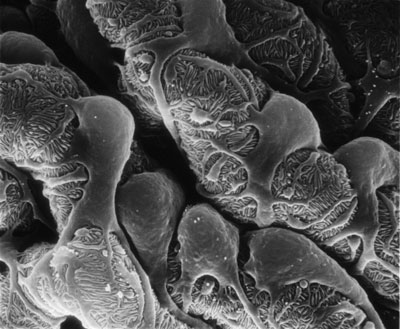
These tiny structures inside the kidney, called glomerular filters, suffer damage from diabetes and grow less effective at filtering the blood. The basic research that led to the clinical trial found that a cell-signaling pathway inside these structures could be a drug target -- and an existing drug being developed for arthritis already targeted that pathway. CREDIT: University of Michigan
It started out as a treatment for arthritis but it could become a first new approach in two decades for treating the damage that diabetes inflicts on the kidneys of millions of people.
University of Michigan Medical School researchers and their colleagues have presented promising results from a clinical trial of the experimental drug baricitinib in people with diabetic kidney disease. In a randomised, controlled Phase II study, it reduced a key sign of kidney damage, with higher doses producing the largest effect, few side effects, and signs of sustained impact even after patients stopped taking it.
U-M researchers not only helped conduct the clinical study – their scientific discoveries set the trial in motion. It’s a fast-track example of the new treatment-development approach known as precision medicine.
The trial results come just three and a half years after the U-M research team linked up with the company that makes baricitinib, Eli Lilly & Co.
That connection resulted from the work of a team led by Matthias Kretzler, M.D. and Frank Brosius, M.D., which had worked for years to pinpoint the importance of a cell-signalling system called JAK-STAT in diabetic kidney disease. By sifting through massive amounts of data on abnormal genetic activity in diseased human kidney tissue, and studying specially bred mice, the team showed JAK-STAT was over-active in multiple kidney cells damaged by diabetes.
Lilly developed baricitinib to calm the inflamed joints of patients with rheumatoid arthritis
But JAK-STAT also plays a key role in diseases where immune-system cells attack normal tissues – such as rheumatoid arthritis. Lilly scientists had developed baricitinib to calm the painful, inflamed joints of rheumatoid arthritis patients, and had received FDA permission to do trials that showed the drug’s safety and impact.
When they learned that Kretzler was scheduled to speak about his research to another group at Lilly, they went to his talk and raised the possibility of using baricitinib against diabetic kidney disease. The international clinical trial, which enrolled 129 adult patients, began quickly – just 14 months after that meeting.
“This is the first example of implementing precision medicine in diabetic kidney disease, which affects 8 million Americans and will surely affect more as the growing diabetes epidemic continues,” says Kretzler. “It shows that the full translational research pipeline is in place, where we can study disease mechanisms, test our findings in model systems, identify drug candidates, find the right partners to take it to a clinical trial, and complete the trial – in 42 months.”
Trial results are the first step in determining if baricitinib or other drugs that act on the JAK-STAT system could fight these effects
The trial showed baricitinib reduced a measure of kidney dysfunction called urinary albumin/ creatinine ratio or UACR, substantially compared with placebo after six months. It also showed that patients had lower levels of two compounds in urine or blood that indicate inflammation in the kidneys, called IP-10 and sTNFR2. The only significant side effect was mild anaemia in the group that received the highest dose, which was expected based on previous research.
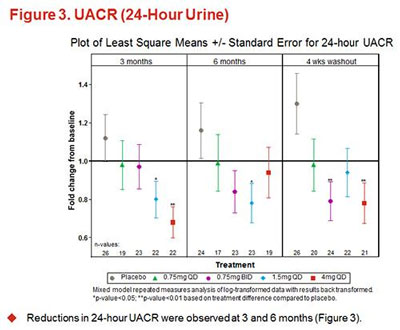
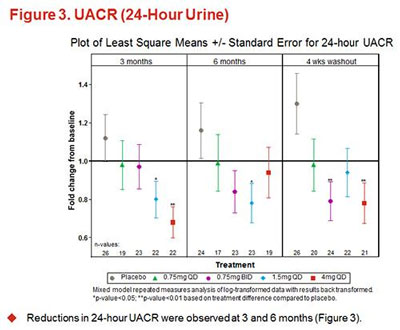
Study results showed that diabetic kidney disease patients taking any of the three tested doses of baricitinib had lower levels of UACR in their urine than patients taking a placebo — even after they stopped taking the drug. UACR is an indicator of kidney function. CREDIT: Bariticitinib trial team
Brosius directed the animal research studies and co-led the multi-institutional clinical trial. He notes that treatment of diabetic kidney disease costs the U.S. billions of dollars yearly. Currently, the standard approach to treating kidney damage in people with diabetes is to control blood pressure using decades-old drugs called ACE inhibitors and ARBs.
“The long-term effects of America’s obesity and diabetes epidemics means that millions more kidneys are at risk. So America urgently needs new approaches to stem the damage that diabetes inflicts on kidney cells,” says Brosius, who heads U-M’s Division of Nephrology and the Michigan Kidney Translational Core Center that helped support this work. “So does the world, as nations like China feel the effects of obesity and diabetes epidemics.”
The new trial results are the first step in determining if baricitinib or other drugs that act on the JAK-STAT system could fight these effects. But they also show promise of combining basic university research, which can uncover specific targets for precise-acting drugs, with drug compounds developed by pharmaceutical companies. Even drugs left on the shelf years ago, or already in use for other diseases, could be tested for new uses based on research findings from teams like the U-M group.