Alzheimer’s drug milestone “bittersweet” for certain patients
Posted: 23 August 2024 | Catherine Eckford (European Pharmaceutical Review) | No comments yet
The first new dementia medicine to be licensed in over two decades shows for first time, that the course of Alzheimer disease can be modified and slow cognitive decline.
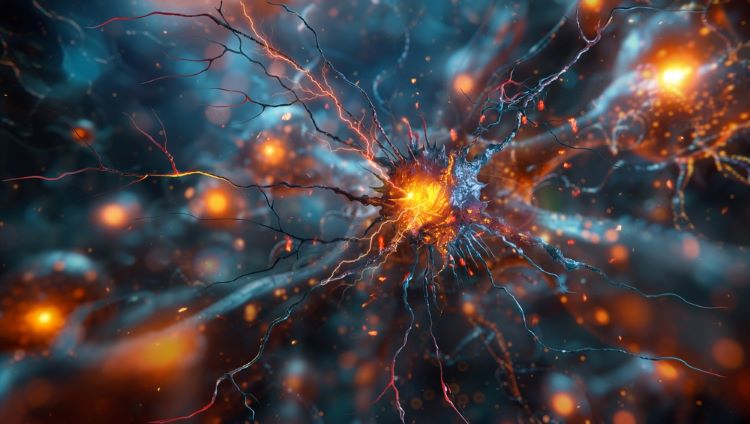
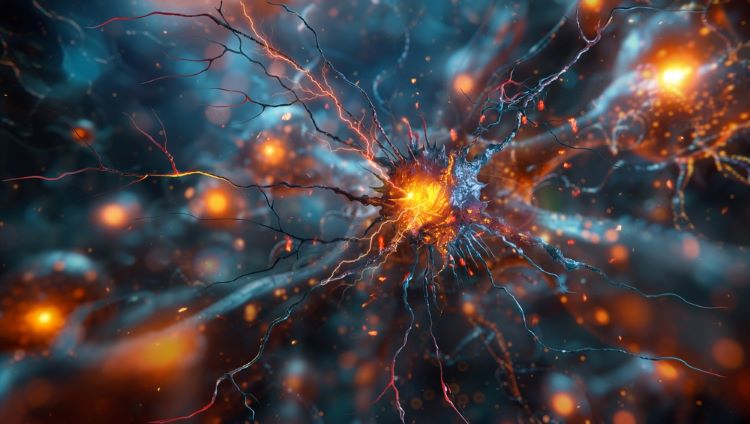
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved the first treatment for Alzheimer’s in Great Britain that has shown some efficacy in slowing disease progression. Lecanemab is authorised to treat adults with early Alzheimer’s.
It is therefore indicated for individuals with either one or no copies of the apolipoprotein E4 gene (ApoE4). They can have no copies, one copy or two of this gene.
“The decision from MHRA to authorise lecanemab is an important step forward for eligible patients in Great Britain”
The Commission on Human Medicines (CHM), the UK government’s independent advisory body advised: “the risk benefit of lecanemab was favourable in the patients who were ApoE4 non-carriers or heterozygous but not in the homozygous group, and that testing for the APOE4 gene should be carried out before treatment”.
The MHRA’s decision is largely based on the Phase III data from the global Clarity AD clinical trial, which demonstrated statistically significant results for participants with Alzheimer’s.
“The decision from MHRA to authorise lecanemab is an important step forward for eligible patients in Great Britain who could now for the first time gain access to a treatment which in studies has been shown to slow the progression of early Alzheimer’s disease,” commented Gunilla Osswald, CEO at BioArctic.
NICE’s decision on lecanemab
However, a draft recommendation issued by the National Institute for Health and Care Excellence (NICE) has deemed that the benefits of lecanemab “are too small” to warrant making the drug available on the NHS.
This is because the anti-amyloid antibody drug “is an intensive treatment to give to patients involving a hospital visit every two weeks with skilled staff needed to monitor them for signs of serious side effects, plus the cost of purchasing the drug,” according to Dr Samantha Roberts, Chief Executive of NICE.
Due to clinical evidence only reporting patients taking lecanemab for 18 months, NICE stated this means there is “a lack of evidence on its long-term effects”.
“Lecanemab provides on average four to six months slowing in the rate of progression from mild to moderate Alzheimer’s disease, but this is just not enough benefit to justify the additional cost to the NHS,” Helen Knight, Director of medicines evaluation at NICE explained.
Public consultation on the draft NICE guidance will end 20 September 2024, NICE confirmed.
Further industry comment
“The combination of high cost of the drug, relatively low impact on disease and significant risk likely justify the NICE guidance. It is possible that, as better ways of identifying those most likely to benefit emerge and the result of longer-term use in the US are revealed, the balance may shift and the guidance change,” Professor Paul Morgan, Interim Director, UK Dementia Research Institute Cardiff, Cardiff University remarked.
“Whatever your view on the decision taken by MHRA and NICE, the key take-away is that lecanemab has been licensed. This is encouraging for the development of next-generation therapies that will provide greater benefit at less risk. There are grounds for optimism that these next-generation drugs will become available on the NHS. It is crucial, therefore, that the UK remains laser-focussed on developing these treatments,” Professor John Gallacher, Director of Dementia Research UK and University of Oxford.
“NICE’s statement does not represent a final decision but the beginning of a period of consultation and the provision of further information,” Professor Robert Howard, Professor of Old Age Psychiatry, UCL Division of Psychiatry, UCL summarised.
Lecanemab is subject to additional monitoring.
Related topics
Antibodies, Biologics, Biopharmaceuticals, Clinical Development, Clinical Trials, Data Analysis, Drug Development, Drug Markets, Proteins, Regulation & Legislation, Research & Development (R&D), Therapeutics
Related organisations
BioArctic, Eaisi, Medicine and Healthcare products Regulatory Agency (MHRA), National Institute for Health and Care Excellence (NICE)
Related drugs
Related people
Dr Samantha Roberts (NICE), Gunilla Osswald, Helen Knight, Professor John Gallacher, Professor Paul Morgan, Professor Robert Howard