Learning from lecanemab: a breakthrough treatment
Posted: 6 March 2023 | Catherine Eckford (European Pharmaceutical Review), Dr Michael Irizarry (Eisai) | 2 comments
Here, Dr Michael Irizarry, Eisai’s Senior Vice President of Clinical Research and Deputy Chief Clinical Officer for Alzheimer’s Disease and Brain Health discusses its highly anticipated Alzheimer’s drug, lecanemab.
With nearly 10 million new cases of dementia of every year1, the increasing prevalence of Alzheimer’s disease (AD), the most common form of the condition, has prompted researchers and the pharmaceutical industry to seek novel, effective solutions.
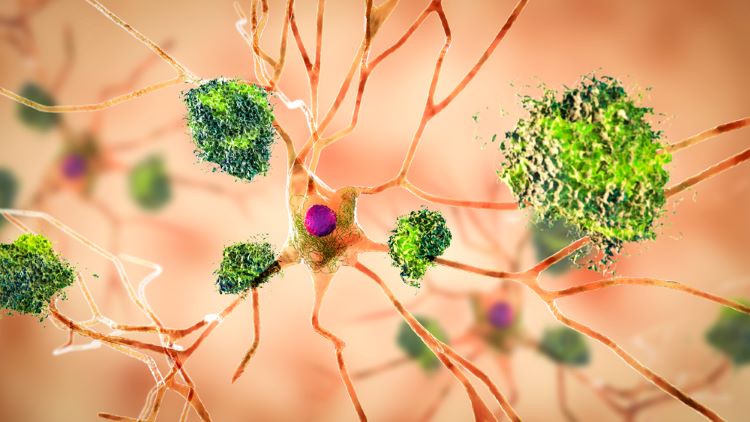
Presence of amyloid beta plaques are one of the hallmarks of AD. Keen to learn more about lecanemab’s promising potential to treat the disease, EPR caught up with Dr Michael Irizarry, Senior Vice President of Clinical Research and Deputy Chief Clinical Officer of Alzheimer’s Disease and Brain Health at Eisai.
January 2023 marked a pivotal turning point for treating Alzheimer’s. Lecanemab, Eisai and Biogen’s anti-amyloid beta (Aβ) monoclonal antibody (mAb) was the subject of numerous regulatory submissions and approvals.
On 6 January, a milestone was achieved—lecanemab gained US Food and Drug Administration (FDA) approval via the Accelerated Approval pathway.
Eisai submitted a marketing authorisation application in Europe for lecanemab for early Alzheimer’s on 10 January 2023. The application was accepted by the European Medicines Agency (EMA) on 26 January, signalling another significant breakthrough for both patients and experts working to address the disease.
This momentum continued, resulting in lecanemab received Priority Review status in Japan several days later, on 29 January 2023.
Recently, on 5 March 2023, the FDA accepted Eisai’s filing of a Supplemental Biologics License Application (sBLA) supporting the conversion of the accelerated approval of lecanemab (leqemibi) to a traditional approval.
Backed by the significant results seen in the pivotal Clarity AD study, Dr Irizarry maintained that unlike other treatments, “lecanemab addresses pathophysiological features of Alzheimer’s disease.”
In addition to laying out some of the key findings from the trial, Dr Irizarry shared the four key factors Eisai deems essential for successful clinical trials.
Why does an anti-amyloid-beta protofibril antibody have potential to treat Alzheimer’s?
In a brain affected by AD, multiple Aβ aggregates exist in complex equilibrium, including dimers, oligomers, protofibrils and insoluble fibrils. Soluble aggregates such as protofibrils are thought to be toxic to neurons. Lecanemab is a humanised antibody generated using protofibrils engineered from Aβ harbouring genetic mutations that cause familial AD.
What were the challenges and the lessons learned when developing lecanemab?
Lecanemab is an antibody that targets Aβ protofibrils, the main abnormal protein of neurotoxicity caused by the Arctic mutation in amyloid precursor protein, one of the causes of familial AD, generating the right hypothesis.
In clinical trials, we targeted the early AD population with confirmed amyloid in the brain and found the right optimal dose that balanced efficacy and safety in the large Phase II dose-ranging study. At Eisai, we believe that the most important factors for successful clinical trials are the four R’s: Right Hypothesis, Right Population, Right Dosage and Right Endpoint.
Building on these 4R’s, we designed the Phase III Clarity AD study in order to definitively assess the safety and efficacy of lecanemab. We believe this is the reason why we were successful with this Clarity AD study.
What sets lecanemab apart from other Alzheimer’s treatments in the current drug approval space?
The previous drugs indicated for AD were symptomatic therapies, whereas lecanemab addresses pathophysiological features of Alzheimer’s disease.”
The previous drugs indicated for AD were symptomatic therapies, whereas lecanemab addresses pathophysiological features of Alzheimer’s disease.
Lecanemab is a humanised IgG1 monoclonal antibody directed against aggregated soluble and insoluble forms of Aβ. The accumulation of Aβ plaques in the brain is a defining pathophysiological feature of Alzheimer’s disease. Lecanemab reduces amyloid beta plaques, as evaluated in Study 201 and Clarity AD.
What can you tell us about lecanemab’s performance in the Clarity AD study?
Lecanemab treatment [reduced] clinical decline on the global cognitive and functional scale, compared with placebo at 18 months by -0.45 (95 percent Confidence Interval (CI): -0.67, -0.23; P=0.00005). This represents a 27 percent slowing of decline.
Lecanemab treatment [demonstrated] a 27 percent slowing of [clinical] decline.”
In the confirmatory Phase III Clarity AD trial, mean change of CDR-SB from baseline at 18 months as the primary endpoint was 1.21 and 1.66 for lecanemab and placebo groups, respectively.
Starting as early as six months (difference: -0.17 [95 percent CI: -0.29, -0.05]; P<0.01), and increasing in absolute difference over time across all time points every three months, the treatment showed highly statistically significant changes in CDR-SB from baseline compared to placebo (all p-values are less than 0.01).
In the amyloid PET sub-study, treatment with lecanemab showed statistically significant reduction in amyloid plaque burden at all timepoints starting at three months.
Lecanemab slowed decline of cognitive function by 26 percent on Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog)14 at 18 months.
In the Alzheimer’s disease composite score (ADCOMS) assessment, lecanemab slowed disease progression by 24 percent at 18 months.
Read the full results of Eisai’s Phase III Alzheimer’s study for lecanemab published in the New England Journal of Medicine (NEJM).
About the authors


Dr Michael Irizarry is the Senior Vice President of Clinical Research and Deputy Chief Clinical Officer, Alzheimer’s Disease and Brain Health, Eisai. He joined Eisai in 2018 as Vice President, Clinical Research for the company’s Epilepsy and Sleep/Wake therapeutic areas. Dr Irizarry spent 12 years as a researcher at the Massachusetts Alzheimer’s Disease Research Center. Since 2006, he has held leadership positions in the neuroscience area at Eli Lilly and in epidemiology at GlaxoSmithKline. Dr Irizarry earned undergraduate and medical degrees from Georgetown University and a Master of Public Health degree from the Harvard School of Public Health.
Catherine Eckford is Editorial Assistant at European Pharmaceutical Review.
References
- World Health Organisation (WHO). Dementia. [internet]. 2022. [cited2023Mar]. Available from: https://www.who.int/news-room/fact-sheets/detail/dementia
Related topics
Antibodies, Biopharmaceuticals, Clinical Development, Clinical Trials, Data Analysis, Drug Development, Drug Safety, Interviews, Proteins, Regulation & Legislation, Research & Development (R&D), Therapeutics










This is nice post thankyou for sharing.
Thanks for providing such information.